University of Pennsylvania researchers have found a promising new treatment for periodontitis using a component of the immune system called complement, according to a new study in the Journal of Immunology (May 7, 2014).
Nearly half of all U.S. adults have periodontitis, and 8.5% of these adults have a severe form that can increase the risk of heart disease, diabetes, arthritis, and pregnancy complications, according to a university press release.
For this study, researchers treated monkeys with a complement inhibitor drug, which successfully prevented the inflammation and bone loss associated with periodontitis, they reported. This treatment could be promising for treating humans with the disease, the researchers concluded.
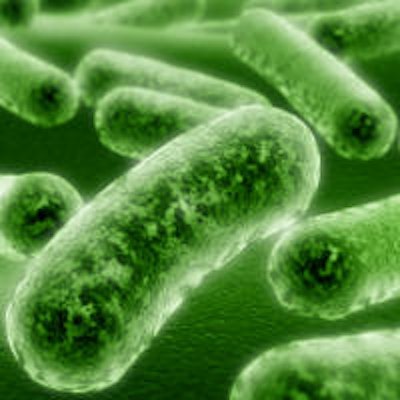
Earlier work by the Penn team had shown that the periodontal bacterium Porphyromonas gingivalis can hamper the ability of immune cells to clear infection, allowing P. gingivalis and other bacteria to flourish and inflame periodontal tissue (J Immunol, December 2012, Vol. 189:11, pp. 5442-5448.
"P. gingivalis has many mechanisms to escape killing by the immune system, but getting rid of inflammation altogether is not good for them because they 'feed' off of it," noted senior study author George Hajishengallis, DDS, PhD, a professor in the department of microbiology in the Penn School of Dental Medicine, in the release. "So P. gingivalis helps suppress the immune system in a way that creates a hospitable environment for the other bacteria."
The researchers wondered which component of the complement system was involved in contributing to and maintaining inflammation in the disease. Their experiments focused on the third component of complement, C3, which occupies a central position in signaling cascades that trigger inflammation and activation of the innate immune system.
The researchers found that mice bred to lack C3 had less bone loss and inflammation in their gums several weeks after being infected with P. gingivalis compared with normal mice. C3-deficient mice were also protected from periodontitis in two additional models of disease: one in which a silk thread is tied around a tooth, promoting the buildup of microbes, and one in which the disease occurs naturally in aging mice, mimicking how the disease develops in aging humans.
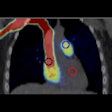
 Complement, a key part of the innate immune system, contributes to gum disease and blocking it can prevent disease. Image courtesy of the University of Pennsylvania.
Complement, a key part of the innate immune system, contributes to gum disease and blocking it can prevent disease. Image courtesy of the University of Pennsylvania."Without the involvement of a different complement component, the C5a receptor, P. gingivalis can't colonize the gums," Dr. Hajishengallis said. "But without C3, the disease can't be sustained over the long term."
The next step was to test a human drug that blocks C3 to see if it reduced the signs of periodontal disease in monkeys (unlike mice, monkeys are responsive to the human drug). Researchers found that the C3 inhibitor, a drug called Cp40, reduced inflammation and significantly protected the monkeys from bone loss. Cp40 was developed to treat the rare blood disease PNH and ABO-incompatible kidney transplantation.
"We think this drug offers a promising possibility for treating adults with periodontitis," said co-author John Lambris, PhD, a professor of research medicine in the department of pathology and laboratory medicine at Penn. "Blocking C3 locally in the mouth helps shift the balance of bacteria, producing an overall beneficial effect."
The study represents the first time anyone has demonstrated the involvement of complement in inflammatory bone loss in nonhuman primates, setting the stage for translation to human treatments, according to the researchers.
The results "provide proof-of-concept that complement-targeted therapies can interfere with disease-promoting mechanisms," Dr. Hajishengallis said.
The research was supported by the National Institutes of Health, the European Commission, and the University of Pennsylvania Institute for Translational Medicine and Therapeutics.