Cone-beam CT and magnetic resonance imaging (MRI) offer a number of advantages over 2D imaging tools for diagnosing temporomandibular disorders (TMD) and orofacial pain, according to a paper in Dental Clinics of North America (July 2013, Vol. 57:3, pp. 405-418).
While as many as 50% of elderly people may be affected by orofacial pain, it is often hard to diagnose, noted the study authors, from the College of Dental Medicine at Georgia Regents University. This is because orofacial pain can be attributed to a variety of disorders, including TMD, odontogenic disease, neuralgia, and headaches.
Of these, TMD is considered to be one of the primary causes of orofacial pain, the researchers noted. Research diagnostic criteria for TMD (RDC/TMD), first published in 1992 and updated in July of this year, detail the clinical and historical assessment of TMD patients. Among other things, the RDC/TMD recommend arthrography and MRI for evaluating disk displacement and tomography for evaluating bony changes.
"Diagnostic imaging, when indicated, is an important part of the examination process for TMD and orofacial pain patients," the researchers wrote.
A number of new imaging techniques have been introduced since 1992, however, which prompted the authors of the present study to consider if some of these newer modalities offer advantages for orofacial pain diagnoses.
For example, the original RDC/TMD and updated RDC/TMD do not list panoramic radiography as an imaging option for TMD assessment, which the researchers speculate may be because panoramic radiographs only depict the lateral poles and central parts of the condyle. However, panoramic x-ray systems can be equipped with a temporomandibular joint (TMJ) imaging program, allowing images to be acquired at a more appropriate angle, they noted.
3D imaging tools
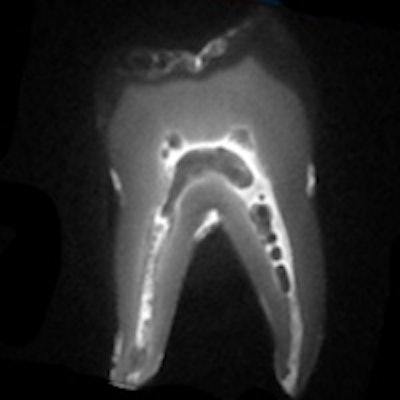
Cone-beam CT's ability to assess details in multiplanar views makes it a "unique tool for accurate and precise valuation of dentoalveolar structures," the researchers wrote. In addition, "the spatial resolution has tremendously improved with the new generation cone-beam CT scanners," which utilize flat-panel detectors rather than image intensifiers and charged-couple devices. The high spatial resolution enables users to evaluate early bony changes in the TMJ, they noted.
In addition, studies have demonstrated that cone-bean CT performs better than conventional tomography, panoramic radiography, and medical CT when evaluating the components of the TMJ, they added -- and often with lower radiation doses.
"In some cases, a TMJ examination acquired with cone-beam CT can be accomplished at one-half the effective dose of an intraoral full-mouth series radiographic examination," the study authors wrote.
Another 3D imaging tool -- MRI, which is nonionizing -- can be used to evaluate the soft-tissue components of the TMJ, they noted.
"MRI has superior soft-tissue differentiation because of its improved contrast resolution over conventional tomography and cone-beam CT," they wrote.
MRI can be used to evaluate the position, shape, and signal of the disk; the presence or absence of fluid within the joint space; the marrow signal of the condyle; the presence of loose bodies within the joint, and osseous changes, the researchers noted. In addition, some research has suggested that MRI be routinely used when evaluating trigeminal neuralgia to rule out potential causes of secondary trigeminal neuralgia (Journal of the American Dental Association, April 1998, Vol. 129:4, pp. 438-447).
Headaches are another indication for using CT, MRI, or both as diagnostic tools, according to the study authors. In particular, a severe headache with sudden onset, a new-onset headache, a migraine of adult onset, cluster headache, or a change in the nature of a headache are all potential indications for brain imaging, they noted.
"Advanced imaging with computed tomography or MRI may be indicated for orofacial pain patients presenting with idiopathic facial pain, headaches, or trigeminal neuralgia," they concluded. "The suspected cause of clinical symptoms would influence the imaging examination ordered."