Esophageal cancer patients who are black and in lower socioeconomic groups have higher mortality rates than white patients with higher incomes, according to a new study presented at the recent meeting of the Society of Thoracic Surgeons in Phoenix.
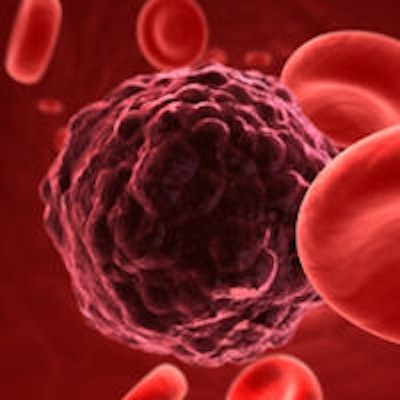
Researchers at Duke University School of Medicine focused on esophageal cancer because it historically has had higher death rates among blacks and a high overall mortality.
The importance of this study for oral healthcare professionals, according to the authors, is the need to be aware of the increased risk for esophageal cancer in black and poor patients.
Esophageal cancer is the 10th leading cause of cancer deaths in the U.S., according to the National Cancer Institute (NCI). There were 16,980 new cases of the disease in 2015, resulting in more than 15,500 deaths, based on NCI statistics. Esophageal cancer is more common in men than women and is associated with older age, heavy alcohol use, and tobacco use. The disease is often diagnosed at an advanced stage, because there are no early signs or symptoms, according to the NCI.
"In lower socioeconomic groups, outcomes for esophageal cancer vary by race, but not in higher socioeconomic groups," said senior author Matthew Hartwig, MD, an assistant professor of surgery at Duke, in a statement. "This has implications for all sorts of cancers, not just esophageal cancer, and should be further examined to eliminate health care disparities."
Lower survival rates
The researchers used the National Cancer Data Base to analyze the records of 16,807 patients, including 6,147 who had surgery (stages I-III) between 2003 and 2011. Of those who had surgery, 5% (293) of patients were black and just over 40% (2,476) of the patients were in the two lowest income brackets. For purposes of this study, patients were grouped using median income by ZIP code, rather than using federal poverty levels.
Before adjusting for income, the researchers reported that black patients had lower overall survival rates than white patients (median survival was 33 months versus 46 months, respectively). Patients with lower incomes were associated with progressively worse survival, the researchers found. The median survival for low-income black patients was 26 months versus 40 months for low-income white patients.
There was no significant difference in overall survival between white and black patients in the two highest income brackets.
Black patients less likely to have surgery
Black patients were also much less likely than white patients to undergo surgery, said lead researcher Loretta Erhunmwunsee, MD. Surgery is part of the combination treatment that is considered optimal, she noted. Dr. Erhunmwunsee is now with the City of Hope in Duarte, CA.
The study found that those patients in lower socioeconomic levels are at a higher risk of death following surgery.
"This disparity likely is based on many factors -- minority patients and patients with lower socioeconomic status often smoke more, have poor eating habits, exercise less, and are exposed to environmental hazards, all of which lead to worse health," Dr. Erhunmwunsee said. Specifically, increased smoking and poor eating habits increase the risk of esophageal cancer, she noted.
"Prior studies have shown that ethnic minority and poor patients who have access to care may still get inappropriate treatment; however, even when they do receive adequate therapy (surgery), as in this study, disparities are prevalent," Dr. Erhunmwunsee said.
Greater awareness in healthcare practitioners of the issue is one of the goals of the study.
"We also hope that awareness of the problem among physicians and patients alike will lead to more public and professional focus on solving this disparity through strategies aimed at health policy, practices of health systems, and training of healthcare providers," Dr. Erhunmwunsee said.