|
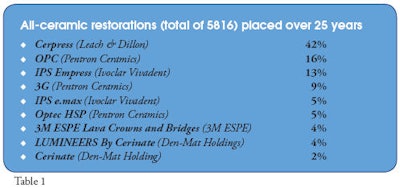
THE DENTAL ADVISOR has documented the placement and monitored nearly 6,000 all-ceramic restorations over the past 25 years. Early on, many of the restorations were one or two units. Today, it is not unusual to restore six, eight, or more all-ceramic units in one appointment.
This issue of THE DENTAL ADVISOR (October 2008, Vol. 25:8) reports on the performance of many of these restorations over time and provides the clinician with insight as to what works and why. Of special interest is the fracture rate of nine all-ceramic materials.
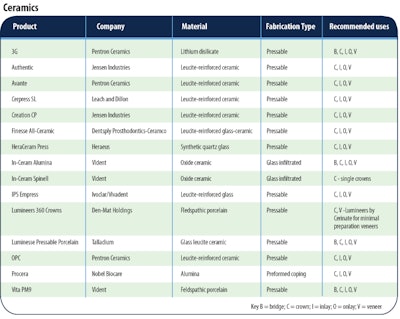
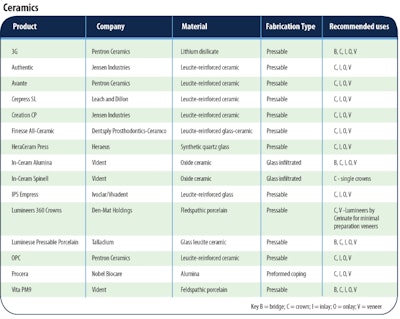
Product Comparison Chart (Click link below to view)Table 3 - Ceramics
[Close chart] Scroll at bottom
Introduction
Over the past 25 years, nearly 6,000 all-ceramic restorations have been placed and monitored by THE DENTAL ADVISOR. Dr. Farah placed restorations during the first 14 years; while during the most recent 11 years, Drs. Farah, Brown, Anderson, and their associates have added more than 4,000 restorations. Table 1 shows the number of restorations placed over that period of time.
All-Ceramic Restorations
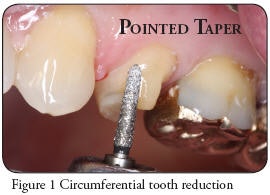
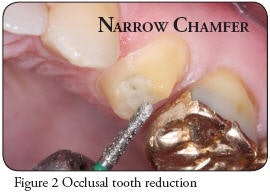
Rules for Good Preparation Design
Fabrication of All-Ceramic Restorations
Flaws in the restoration such as internal cracks, weakening of the material because of heating and cooling cycles, improper layering of the ceramic, and contour and anatomy are reasons an all-ceramic restoration can fail. Using the required firing and cooling temperatures of the material and the proper layering technique of the ceramic will strengthen the restoration.Internal cracks in the ceramic can develop during the firing and cooling process and in building the external layers of ceramic. Use of a trans-illuminating light (Microlux/AdDent, Inc.) on the intaglio side of the restoration will show internal flaws and cracks that are not always visible to the naked eye. If cracks appear, return the restoration to the laboratory. Patient occlusion can also contribute to the failure of an all-ceramic restoration. Patients that are heavy bruxers or have restorations with improper occlusion can put tremendous force on a restoration causing catastrophic failure. Bonding or Cementation of All-Ceramic Restorations
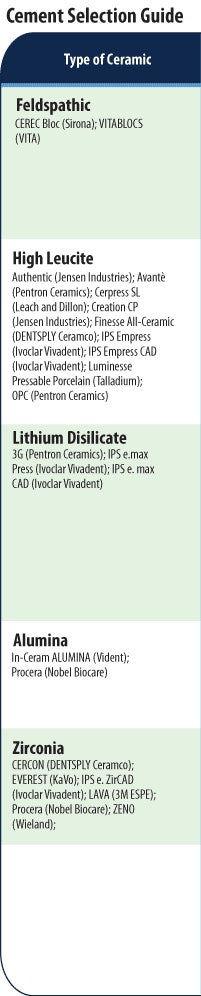
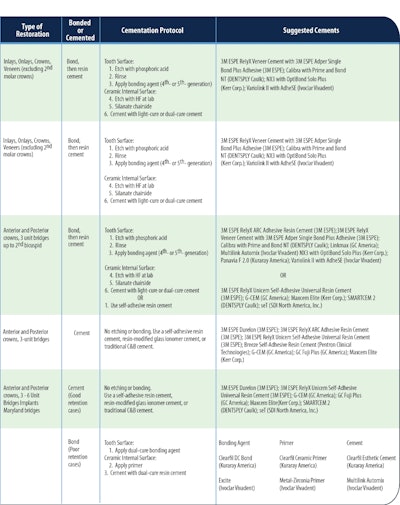
High-leucite all-ceramic restorations should be bonded using a bonding agent and resin cement (see Table 2). Lithium disilicate and alumina restorations can be bonded or cemented with self-adhesive resin cement in selected cases. All-ceramic products are listed in Table 3. Performance of All-Ceramic Restorations Over 25 Years
Failures as a Function of Time
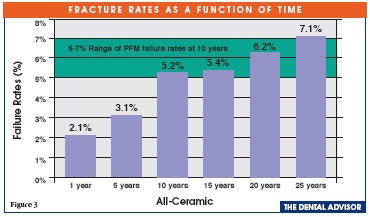
Fracture rates ranged from 2.1% at one year to 7.1% at 25 years. Over time, restorations will weaken, regardless of the material used. Figure 3 illustrates the fracture rates of all-ceramic versus PFM restorations. Many dentists and laboratories believe that metal is stronger than all-ceramic. However, our data show the failure rate of all-ceramic restorations at 10 years to be slightly less than the failure rate of PFM. In recent years, the cost of all-ceramic restorations has aligned with the cost of PFM due to an increase in the cost of precious metals.
Fracture and Chipping
There are many reasons why all-ceramic restorations fracture or chip. Top Five Reasons for Fracture
Marginal Staining
Marginal staining is noted by the graying margins of anterior and posterior crowns and veneers. Marginal staining is rarely noted for inlays and onlays, but occurs in 5.5% of other all-ceramic restorations at 10 years. The graying is unattractive to patients and is the most frustrating factor pertaining to cosmetic restorations, often occurring within days of cementation. Using a zirconia coping under a ceramic overlay masks the graying. Possible causes of marginal staining are:
Debonding
It is not always easy to determine if the bond failure is at the tooth/resin or resin/ceramic interface. Most often it seems to be related to both interfaces. Inlays have a much lower debonding rate, less than 1%. Wear Resistance
Aesthetics
All-ceramic restorations are designed with extraordinary aesthetics in mind. Factors such as tooth staining and dark posts or cores can dramatically affect the overall final appearance and shade of the restoration. In recent years, aesthetic post systems and tooth-colored core materials have been developed to assist dentists in attaining excellent aesthetic results. Checklist for Success - Communicating With Your Laboratory
The dentist and the laboratory must have open communication and awareness of the limits of the material. These are the items you should send to the laboratory with each all-ceramic restoration request. Your preparation and clear communication with your laboratory will result in excellent aesthetics.
All-Ceramic Restorations: The Next 10 Years
Trends in all-ceramic restorations are moving to exciting and new areas. Digital workflow and chairside CAD/CAM fabrication allow instant feedback for the dentist and laboratory. Our November 2008 issue of THE DENTAL ADVISOR will focus on the basic principles of CAD/CAM, the introduction of zirconia restorations, and the integration of digital dentistry into daily practice for laboratories and dentists. Requests for reprints should be directed to The Dental Advisor. |