Administering amoxicillin and metronidazole immediately following periodontal surgery can significantly reduce the need for additional surgery, according to researchers from the University of Geneva School of Dental Medicine.
In a presentation at the recent International Association for Dental Research (IADR) meeting in Toronto, Norbert Cionca, D.D.S., assistant in the department of periodontology at the university, shared results from a six-month double-blind randomized study of patients with chronic periodontitis. The goal was to determine whether antibiotics enhance the effects of full-mouth debridement and deter the need for follow-up surgery.
"There have been numerous studies that examined the effect of different regime antibiotics on clinical and microbiological parameters of periodontal diseases," Dr. Cionca said in an e-mail interview with DrBicuspid.com (for example, Journal of Clinical Periodontology, October 2005, Vol. 32:10, pp. 1096-107 and March 2007, Vol. 34: 3, pp. 243-253). "The problem was some were not randomized or controlled, the antibiotics used were different between studies, and the definition of the periodontal disease changed from one to another."
In the University of Geneva study, 47 patients ages 25 to 70 were followed for six months. These patients each had received a prior diagnosis of adult chronic periodontitis, with at least four teeth having a probing pocket depth of at least 5 mm, clinical attachment loss of at least 2 mm, and radiographic evidence of bone loss. Forty patients received full-mouth periodontal debridement.
Within 48 hours of surgery, 20 subjects began a treatment regimen of 500 mg of metronidazole and 375 mg of amoxicillin, three times a day for seven days. The other 20 received a placebo.
"A combination of antimicrobial drugs may have a wider spectrum of activity than a single agent," Dr. Cionca noted. For patients who cannot tolerate amoxicillin, the use of cefuroximaxetil or ciprofloxacin has been suggested, he added.
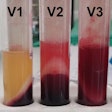
A total of 3,126 sites (six per tooth) were clinically monitored at baseline, three months, and six months. Each tooth was assessed on plaque index (PI), gingival index (GI), probing pocket depth (PPD), recession (Rec), bleeding on probing (BoP), and adverse events (see table, below).
|
||||||||||||||||||||||||||||
| n.s. = nonstatistically significant All data courtesy of Dr. Norbert Cionca. | ||||||||||||||||||||||||||||
After six months, mean PPD was significantly lower in the test group than the control subjects (2.9 ± 0.2 mm versus 3.1 ± 0.3 mm). More important, test subjects had a significantly lower mean number of persisting pockets greater than 4 mm PPD and bleeding upon probing. The most important finding, according to Dr. Cionca, was the difference in BoP between the placebo group and those who received the seven-day antibiotic regimen (see table, below).
|
||||||||||||||||||||||||||||||||
| *The difference in attachment level between 6 months and baseline. Attachment level was calculated on the basis of probing pocket depth and recession. | ||||||||||||||||||||||||||||||||
A small number of patients experienced adverse events, with slightly more in the test group suffering nausea, vomiting, and diarrhea. More notable, Dr. Cionca pointed out, was that two members of the placebo group experienced periodontal abscess and two others experienced tooth loss, while none of the test group experienced either (see table, below).
|
"It is clear that the use of these antibiotics significantly improved the clinical outcomes of full-mouth, nonsurgical periodontal debridement and significantly reduced the need for additional surgical therapy," Dr. Cionca concluded.
The study was well-received by the IADR audience. Donald Tanenbaum, D.D.S., M.P.H., of Toronto noted that the findings are important because antibiotics are not well-adopted by general practitioners at this time.
Dr. Cionca agreed. "There is a general consensus that whenever possible, antibiotics should not be administered before completion of a root-surface debridement," he told DrBicuspid.com. "Patients with acute signs of disease such as periodontal abscesses or acute necrotizing gingivitis, with fever and malaise, may be the exception. Systemic antibiotics, given after scaling and root planning, provide an additional treatment benefit, especially in deep pockets, and reduce the need for further surgical therapy. In most cases, however, mechanical therapy is initially carried out without antibiotics and evaluated after an appropriate period of time."
Dr. Cionca and his colleagues plan to publish additional one- and five-year follow-up data, he said. They are also preparing another study to look at the timing of giving antibiotics in periodontal therapy.