After corrective jaw surgery for facial deformities, determining if the necessary skeletal changes have taken place has been difficult for practitioners. A study in PLOS One found that a new method of radiographic measurement using 3D images to assess the maxillomandibular changes after surgery may offer a solution to this issue.
The four methods currently available all have specific limitations, which makes quantifying the changes in the jaw bone after surgery difficult at best. The authors looked at a fifth method, directly landmarking 3D Digital Imaging and Communications in Medicine (DICOM) images, to see if this method could be clinically useful (PLOS One, August 7, 2015).
An accurate method of measurement is needed when practitioners are superimposing 3D images to measure any changes in facial structure, wrote senior study author Ashraf Ayoub, BDS, MDS, PhD, in an email interview with DrBicuspid.com. Dr. Ayoub is a professor of oral and maxillofacial surgery at the University of Glasgow Dental School in the U.K.
"What inspired the study is the need for an accurate method to superimpose 3D images of the face to quantify changes due to surgery, facial growth, or any other reason," Dr. Ayoub wrote.
Accuracy issues
There are four main groups of techniques for assessing skeletal changes:
- Cephalometeric analysis
- Principal component analysis
- Volumetric changes
- Color error maps
Cephalometric analysis, while used routinely to evaluate sagittal changes in maxillary and mandibular position, has the issues of landmark placement and accuracy of the 3D surface model, according to the study authors. Principal component analysis is "complicated for routine use," while the volumetric changes method cannot quantify postoperative positional changes, they wrote. The major drawback to the color error maps method is that it measures the shortest distance "between vertices of adjacent meshes," which may not represent "corresponding anatomical points," according to the authors.
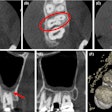
Given the shortcomings of the other methods, the clinical challenge is to measure the accuracy and reproducibility of directly landmarking DICOM image slices and to quantify the positional change of the maxilla and the mandible following simulated orthognathic surgery.
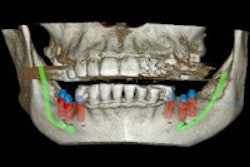
In this study, the researchers used a plastic skull model to simulate the surgical movements and also produce a reference measurement set. They set a total of eight landmarks, three in the maxilla and five in the mandible, before acquiring the images.
The landmark positions were designed to "assess the three-dimensional orientation and movements of the maxilla and mandible," the authors wrote.
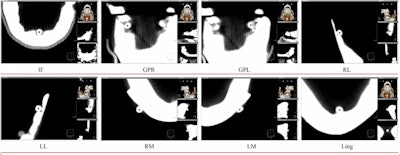
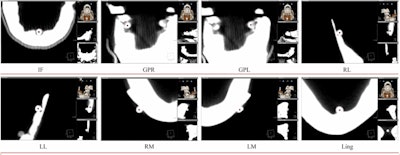
Eight landmarks placed on the DICOM image slice and viewed in 3D: (A) Incisive foramen (IF). (B) Greater palatine right foramen (GPR). (C) Greater palatine left foramen (GPL). (D) Right lingual foramen (RL). (E) Left lingual foramen (LL). (F) Right mental foramen (RM). (G) Left mental foramen (LM). (H) Lingual tubercle (LING). Almukhtar A, Khambay B, Ayoub A, et al. (2015) "Direct DICOM Slice Landmarking" A Novel Research Technique to Quantify Skeletal Changes in Orthognathic Surgery. PLOS One 10(8): e0131540. doi:10.1371/journal.pone.0131540.
After examining the images, the researchers reported a "significant correlation" between DICOM and the present gold standard in the y- and z-directions (r = 0.999, p = 0.0001), (r = 0.998, p = 0.0001), but in the x-direction there was no significant correlation (r = 0.000, p = 0.500).
Further, the results reported a highly significant correlation between the repeated readings for intra- and interexaminer error test in all three dimensions (labeled x, y, and z).
"The lack of statistical difference is a confirmation that [this method is] accurate from the mathematical point of view," Dr. Ayoub stated.
Reliable and reproducible
The authors discussed the issue with finding no significant correlation in the x-direction, writing that it was not possible to measure rotational and lateral movements directly on the plastic skull; therefore, movement in the x-direction was considered to be close to zero throughout the calculations.
"However, the small inadvertent lateral or rotational changes in the x-direction led to the expression of a significant p-value and low correlation when compared to the physical movement in the x direction," the authors wrote.
Despite the x-direction issue in the model, direct DICOM slide landmarking was a valid technique for quantifying these changes, according to Dr. Ayoub and colleagues.
"It promises a reliable and a reproducible 3D surface landmarking to measure surgical changes," they wrote.
Dr. Ayoub continued that thought, writing that oral surgeons should know that internal landmarking of DICOM image slices can be used reliably for clinical applications.