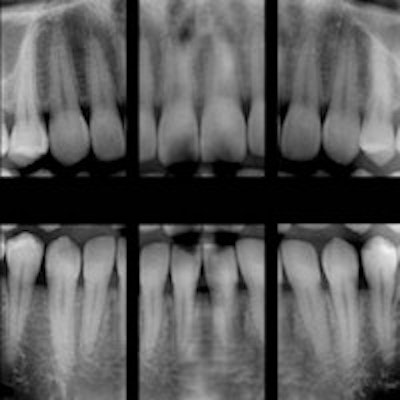
Whether a vertical root fracture (VRF) is complete or incomplete can be difficult to diagnose. Now, the authors of a new study in the Journal of Endodontics ask, if a practitioner is trying to determine if a VRF is incomplete, is digital radiography (DR) or cone-beam CT (CBCT) the better modality to use?
Researchers from the department of endodontology at Kings College Dental Institute and the department of biomedical statistics at the Dental Institute, Denmark Hill, in London, raised the question of which modality is preferred because incomplete root fractures are notoriously difficult to diagnose, and a VRF is usually "associated with a poor prognosis of the affected tooth" (J Endod, October 2014, Vol. 40:10, pp. 1524-1529).
They noted that it is difficult to reach a definitive diagnosis on the basis of signs and symptoms alone because they are not specific to fractures and are very similar to endodontic or periodontal disease. Previous studies examined more than 850 endodontically treated teeth over a five-year follow-up period and reported that of the 64 teeth that required extraction, VRF was identified as the cause in more than 30% of the teeth.
The new study included 21 unsalvageable teeth from 20 patients, the teeth had been radiographed and imaged with CBCT. These teeth were extracted atraumatically and inspected under a microscope to confirm the presence or absence of fracture. Using an optical coherence tomography scanner, the widest point of each fracture was recorded to quantify the size of fractures.
The researchers then asked 13 examiners to view the images under standardized conditions. This process was repeated two weeks later to assess the examiners' consistency.
The results showed that both DR and CBCT imaging showed similarly poor sensitivity (0.16 and 0.27, respectively) and similarly high specificity (0.92 and 0.83, respectively). The researchers found that there was no statistical difference between the diagnostic accuracy of either imaging modality. They also determined that fracture width did not affect the detection rate of either imaging modality.
In this study, there was no significant difference in the diagnostic accuracy of either imaging modality between cases with fracture widths of less than 300 mm and 300 mm or more. The sensitivities of both modalities were significantly less in unfilled teeth (0.0 for DR and 0.05 for CBCT imaging) compared with root-filled teeth (0.33 for DR and 0.11 for CBCT imaging), the study authors noted. However, they caution that the data need to be interpreted with care because of the low number of unfilled teeth (n = 5) compared with root-filled teeth (n = 17).
While previous studies noted that CBCT imaging was more accurate in detecting 0.2- and 0.4-mm fractures compared with DR, the current study authors also noted that in the clinical setting, fractures of 0.4 mm or greater would likely be diagnosed based solely on clinical findings, and a CBCT may, therefore, not be indicated.
Both digital radiography and CBCT have significant limitations when detecting vertical root fractures, and the overall diagnostic accuracy of both imaging modalities was below the accepted threshold suggested in other studies, the authors concluded.
They suggested that the high specificity seen in both modalities means both can reliably detect an unfractured tooth. But, this specificity may also indicate that neither imaging modality is capable of accurately detecting fractures and might be producing a disproportionately high number of negative results.