
Millions of children enrolled in Medicaid in California, Indiana, Louisiana, and Maryland are not getting required dental care, according to a new report from the U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG). The report also provides recommendations on how the states can move forward.
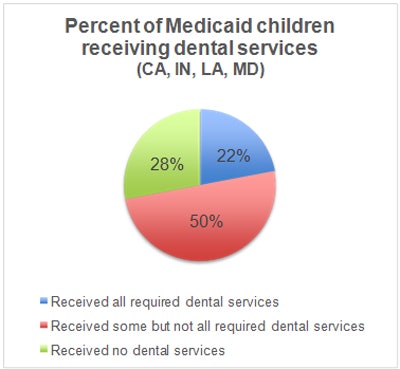
In the report, the OIG looked in depth at whether Medicaid children in those four states were getting biannual oral exams, dental cleanings, and fluoride treatments. The researchers found that 78% of children were not getting the required care needed and also that 28% of children didn't see a dentist at all.
"The states we reviewed reported facing shortages of participating dental providers and challenges in educating families about the importance of regular dental care," wrote Suzanne Murrin, deputy inspector general for evaluation and inspections at HHS. "While the states reported that they employ a variety of strategies to address these problems and the U.S. Centers for Medicare and Medicaid Services (CMS) has taken some positive steps in this area, we continue to have concerns that children are not receiving required dental services."
Why is this important?
Medicaid's Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit requires states to cover all necessary treatment for children, including preventive treatment, but some children are unable to access these benefits. To see if states were actually meeting the required care, the OIG researchers analyzed Medicaid dental claims in four states between 2011 and 2012. They also reviewed beneficiary enrollment files and conducted interviews with state officials.
While visiting a dentist is crucial to maintaining optimal oral and overall health, millions of children enrolled in Medicaid have trouble getting dental care. This sometimes has drastic consequences, as was the case for a 12-year-old boy in Maryland who died after his family could not find a Medicaid dentist to treat his tooth pain, the report noted.
The HHS specifically chose California, Indiana, Louisiana, and Maryland, because those four states adopted the periodicity schedule from the American Academy of Pediatric Dentistry (AAPD), which suggests children receive oral services at a minimum of every six months. Combined, the four states serve nearly 20% of all children enrolled in Medicaid.
What did the report find?
The most prominent report finding was that an average of 78% of children did not receive the dental care required by EPSDT. The exact percentage varied among the four states, with a high of 81% of Louisiana kids not receiving the required care and a low of 73% of kids in Maryland.
 Data courtesy of "Most Children With Medicaid in Four States Are Not Receiving Required Dental Services," January 2016.
Data courtesy of "Most Children With Medicaid in Four States Are Not Receiving Required Dental Services," January 2016.The researchers also found that 28% of children, more than 1 million children in the four states, did not receive any dental care between 2011 and 2012. An additional 14% of children only had one dental visit during the same time period.
Other report findings include the following:
- Children ages 3 and younger were the least likely age group to receive dental care.
- 86% of children who received all required dental care visited the same practice throughout the two years.
- Two states (unnamed in the report) had payment policies that conflicted with their required schedules.
- All four state officials noted a key barrier to dental care for Medicaid children was a lack of providers, typically because of low reimbursement rates or administrative burdens.
How can states move forward?
The reported ended with eight recommendations for CMS and the four states to implement when moving forward:
- Develop a comprehensive plan to increase the number of children who receive required services.
- Develop benchmarks for dental services and require states to create mandatory action plans to meet them.
- Work with states to identify areas with limited providers and the barriers preventing providers from participating in Medicaid.
- Work with states to analyze the effects of Medicaid payments on access to dental providers.
- Work with states to educate families about the importance of dental care and to encourage ongoing relationships between children and their dentists.
- Work with states to track children's utilization of required dental services.
- Identify and share effective strategies.
- Ensure that states pay for services in accordance with their periodicity schedules.
CMS has already reviewed the recommendations in the report, agreeing partially or fully with all but one recommendation -- work with states to track children's utilization of required dental services. The recommendation specifically points out that the data being collected by CMS's Form 416 does not provide enough important information, but CMS disagreed.
"We recognize that CMS has already taken some steps toward addressing the issues we found in this report. It has developed materials to educate consumers and providers about positive oral health practices, and it has shared strategies with states to improve access to and utilization of dental care," Murrin concluded. "However, we continue to have concerns that children are not receiving required dental services."



















