When working with implant patients, dental professionals should identify possible peri-implant disease risk factors, establish a radiographic baseline at the time of implant placement, and continually monitor the implant's health, intervening early if inflammatory complications arise, according to a report in the Journal of Periodontology (April 2013, Vol. 84:4, pp. 436-443).
The paper was developed by an expert committee appointed by the American Academy of Periodontology (AAP) and reviewed and approved by the AAP Board of Trustees in an effort to review the current knowledge of peri-implant mucositis and peri-implantitis, and guide dental professionals in their diagnoses and disease prevention.
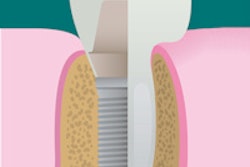
Both peri-implant mucositis and peri-implantitis are characterized by an inflammatory reaction in the tissues surrounding a dental implant that can lead to tissue destruction and, ultimately, implant failure. Peri-implant mucositis is confined to the soft tissue with no sign of supporting bone loss. Peri-implantitis, similar to periodontitis, results in inflammation around the soft tissue and progressive bone loss. Additionally, peri-implant mucositis may be successfully treated using nonsurgical efforts if detected early, whereas peri-implantitis usually requires surgical treatment.
"Although there are widespread clinical reports where dental implants have achieved long-term success, it is important for dental professionals to understand that peri-implant mucositis or peri-implantitis may arise from a failure to identify risk factors, improper treatment planning, suboptimal surgical or prosthetic execution, and/or improper maintenance care," stated Paul Rosen, DMD, chair of the AAP Task Force on Peri-Implantitis, in a news release. "We can't ignore the reality that patients could be suffering from peri-implant mucositis or peri-implantitis and should continually work towards understanding the disease, treatment, and contributing risk factors."
The report outlines numerous key components to aid clinicians in understanding the disease, including disease background, diagnoses, prevalence and incidence, etiologies and pathogenesis, risk factors (including previous periodontal disease, poor plaque control, residual cement, smoking, genetic factors, diabetes, and occlusal overload), and suggested routine following diagnosis.
"Because evidence suggests that early diagnosis and treatment leads to optimal treatment outcomes, regular monitoring of dental implants as part of a comprehensive periodontal evaluation and proper maintenance is crucial to a patient's implant health," noted AAP President Nancy Newhouse, DDS, an assistant clinical professor at the University of Missouri - Kansas City School of Dentistry.