DrBicuspid.com is pleased to present the next column from two lawyers who spend every day defending dentists in litigation and before the licensing board. The purpose of this column is to offer our readers a fresh perspective on common practice and risk management issues from attorneys who litigate these issues in the real world.
A 47-year-old woman who worked as a professional photographer -- mostly doing weddings and other large parties -- was treated for decades by her general dentist; her only ongoing issue was periodontal disease, which initially manifested with generalized 4- to 6-mm pockets, and later progressed to deeper pockets with moderate generalized vertical bone loss. About four years before the subject incident, the dentist referred the patient to a periodontist to best maintain her teeth for as long as possible.
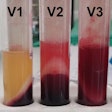
The patient routinely presented every three months to the periodontist for scaling and curettage procedures, and she also underwent two pocket-reduction procedures. At various times over the treatment period, the patient had purulent discharge from her gingival sulcus at different locations. She maintained her regimen of brushing twice daily and flossing once daily, and always advised the periodontist when there had been the sulcular discharge. On certain visits, most particularly when the patient had described recent purulence, antibacterial rinses were prescribed.

At the patient's final visit to the periodontist, she presented with active purulent discharge, which was seen by the periodontist; the periodontist's hygienist noted many 6- to 8-mm pockets during examination, so the dentist gave local anesthesia to the patient so that the hygienist could do deep scaling and curettage. The patient was sent home after the procedure and asked to return in a month for a follow-up; no other instructions were given nor measures taken.
Eight days later, while the patient was home watching television, she experienced a seizure -- the first of her life -- which led to her being transported to a regional medical center; her state of consciousness was altered, so she was kept in the hospital for a neurological evaluation. In the workup, brain radiological studies demonstrated the presence of an intracranial fluid accumulation, which was determined to likely be either blood or pus. An emergency craniotomy was performed, draining a significant amount of pus from what was diagnosed as a brain abscess; culture and sensitivity testing isolated Treponema denticola, which is a bacterial species found almost exclusively in the mouth, especially in periodontal disease lesions.
Following the surgery, the patient was placed on broad-spectrum, intravenous antibiotics until the bacterium was isolated, and then a penicillin derivative to which the bacterium was sensitive was substituted. The patient spent more than two weeks in the hospital, followed by a month of physical and occupational therapy rehabilitation to address deficits associated with the impingement of the abscess upon brain tissue as well as the effects of the surgery.
Ultimately, general recovery was reasonably good, but she lost some executive functions and, because of a sense of imbalance, she could never again climb onto the ladders she had always used to get elevated photography shots; this caused her to end her career as a professional photographer. She took on other jobs that were more sedentary, but her loss of income was significant and provable.
Legal stance
The patient became a plaintiff when her attorney filed an action against the periodontist, claiming that he was negligent in failing to detect the presence of infection and failing to adequately treat it as part of his periodontal treatment, thereby permitting the involved bacteria to travel to the brain and grow, leading to surgery and permanent disabilities.
As the case progressed, it became clear that the plaintiff's attorney's approach was that the periodontist should have given antibiotics to the plaintiff at the time of treatment, due to the presence of an acute infection, demonstrated by purulent discharge.
Issues raised
Despite the severity of the infection and the serious impact it had on the plaintiff, the dentolegal issues are simple and straightforward:
Use of antibiotics: There may be as many views on the question of whether antibiotics are needed in the presence of treatment with an ongoing active infection as there are antibiotics on the market. The general approach most frequently employed in the medical community these days is to minimize antibiotic use so as to minimize the risk of developing resistant bacteria, which become very difficult to manage. Even the traditional preventive uses for antibiotics in dentistry (heart valve anomalies, joint prostheses) have greatly decreased, in large part because of scientific studies that have found the risk of infection at the time to be less than the greater risk of developing "superbugs."
However, this case is not one of preventive or prophylactic use, but instead involves an acute purulent infection requiring antibiotic coverage if invasive dental care will be taking place within the area of that infection. Based on consultations undertaken with dentists and specialists in infectious diseases, the most pervasive line of thought was that prophylactic use of antibiotics -- when no actual infection is present, but rather when the goal is to prevent an infection from developing and potentially spreading -- is shrinking, although it needs to be considered for each specific situation. On the other hand, many practitioners view an actual, acute infection differently: Treatment should be directed at controlling an acute infection before intervening surgically, when possible; if that is not possible, then antibiotics should be provided at the time of or immediately following the intervention. Once again, we repeatedly found practitioners avoiding cookie-cutter tactics for this issue, but instead taking a case-by-case approach.
We took away from our discussions with experts that any of these approaches, especially when looked at in hindsight, can be criticized, so we take this opportunity to express the importance of dentists having solid reasoning for all aspects of their patient care, before any complications occur.
The medical cause of the infection: The hospital record left no doubt that the bacteria that caused the brain abscess originated from the mouth and traveled vascularly to the brain. (We point out that in order for a case in malpractice to be successful, a plaintiff must prove that negligence in a procedure caused an injury.)
The hospital record clearly spoke to the conclusion that the procedure was the causal basis for the bacterial spread, but it said nothing as to whether there was any dental negligence. This set up our defense to focus almost exclusively -- or at least primarily -- on whether there was negligence and to focus less on the cause of the brain abscess or its effects, which all would agree were quite severe.
Deposition testimony: The one critical issue of the periodontist's testimony was whether there was a need for antibiotics to have been prescribed, either before or immediately following the scaling and curettage. Of course, the periodontist testified that, in his opinion, there was absolutely no need for antibiotics in this situation. But when asked for the definition of periodontitis, he stated that it is an infection of the tissues surrounding and supporting the teeth, and he agreed that the presence of purulence defined that infection as acute.
Result
The case was settled significantly below the dentist's policy limits on the eve of trial for reasons discussed below.
Practice tips
We believed that a jury would undoubtedly conclude that the brain abscess arose from bacteria from the mouth, and the lost earnings claim alone could have amounted to the limits of coverage, without even considering the pain and suffering component.
So, it left concern, with the only factor likely up for real discussion in the jury room being whether the periodontist should have ridded the infection before intervening with instruments that create bleeding. We felt secure that our expert would set out a strong argument for judicious use of antibiotics, but we felt equally secure that the plaintiff's expert would strongly argue that an admitted acute infection needed to be managed and controlled before the periodontist set up a situation for spread to a dangerous area.
Risk management tip
Decisions on whether to settle or take the case to verdict are often cloudy, because most dentists generally practice according to proper standards and less-than-ideal results come about even when proper care was supplied; however, part of our function is to fairly consider the risks, and one we consider is the potential for a verdict exceeding policy limits, which would possibly put personal assets at risk.
Here, in conjunction with the client, the decision was made to reach a known result. "Better the devil you know than the devil you don't know."
William S. Spiegel, Esq., is a partner at the law firm Spiegel Leffler in New York City. He is a former assistant corporation counsel to the City of New York -- Medical Malpractice Division.
Marc R. Leffler, DDS, Esq., is also a partner at Spiegel Leffler. He received his dental degree from Columbia University, completed a residency in oral and maxillofacial surgery at New York University, and is a diplomate of the American Board of Oral and Maxillofacial Surgery.
Disclaimer: Nothing contained in this column is intended as legal advice. Our practice is focused in the state of New York, and there are variations in rules of practice, evidence, and procedure among the states. This column scratches the surface on many legal issues that could call for a chapter unto themselves. Some of the facts and other case information have been changed to protect the privacy of actual parties.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.