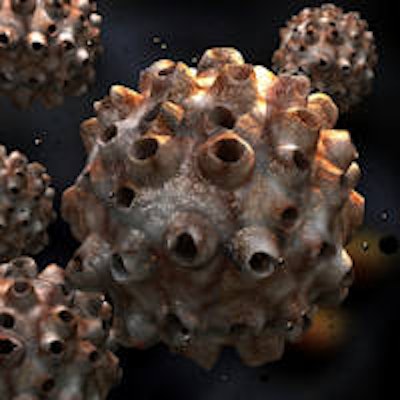
Human papillomavirus type 16 (HPV16) antibody status, particularly for E antibodies, is a strong predictor of survival among patients with HPV-positive oropharyngeal squamous cell carcinoma, according to a study in Clinical Cancer Research. Specific antibody status can be used to identify patients with HPV16-positive tumors who may benefit from altered monitoring and treatments.

Patients who had E antibodies had better overall and progression-free survival rates than patients who did not (Clin Cancer Res, June 15, 2015, Vol. 21:12, pp. 2861-2869).
"If serologic positivity to E antigens has some survival advantage, then you would want to do something to generate a greater humoral immunity (antibody response)," senior author Erich Sturgis, MD, MPH, told DrBicuspid.com. "This would typically be a vaccine approach." Dr. Sturgis is a professor in the department of head and neck surgery and the department of epidemiology at the University of Texas MD Anderson Cancer Center.
Growing incidence
The incidence of HPV-positive oropharyngeal squamous cell carcinoma has increased greatly in recent years, the study authors noted.
The incidence of HPV-positive oropharyngeal cancers increased by 225% from 1988 to 2004 (from 0.8 per 100,000 to 2.6 per 100,000). If this trend continues, the annual number of HPV-positive oropharyngeal cancers is expected to surpass the annual number of cervical cancers by the year 2020 (Journal of Clinical Oncology [JCO], November 10, 2011, Vol. 29:32, pp. 4294-4301).
The number of such cases is expected to rise significantly over the next decades because of a lack of a screening paradigm and despite the availability of a prophylactic vaccine, noted the authors of the 2011 JCO study.
Serum antibodies to HPV proteins, in particular the early (E) proteins E6 and E7, have been detected in several HPV-related cancers and have been reliable indicators of an HPV-positive tumor, including oropharyngeal tumors. Many studies have shown that patients with HPV-positive tumors respond better to treatment and have better survival than patients with HPV-negative tumors.
Serologic immune responses to HPV16-positive tumors may correlate with high viral load, the current study authors noted. For example, in a Costa Rica HPV16 vaccine trial, high viral load could predict the presence of HPV16 antibodies in 646 young, HPV16-infected women (BMC Infectious Diseases, August, 11, 2010, Vol. 10:238).
In the current study, U.S. researchers used a novel protein array to investigate the biologic and prognostic relevance of serum antibodies related to such patients at the MD Anderson Cancer Center in Texas.
| Study patient characteristics | ||
| Patients (209 total) | 184 men | 25 women |
| HPV16 status (114 patients) | 96 positive | 18 negative |
| Smokers for more than 10 years | 78/209 | |
| E antibodies | 90% | |
| L antibodies | 15.8% | |
| NE2 antibody | 82.8% | |
| CE2 antibody | 48.3% | |
Median follow-up was about five years (62.7 months) for all surviving patients and nearly six years (68.9 months) for surviving patients with HPV16-positive tumors.
Impact of key antibodies
A greater proportion of patients who were positive for any E antibodies had better five-year overall survival rates (87.4% versus 42.2%) and five-year progression-free survival rates (82.9% versus 46.1%) than patients who were negative for E antibodies (p < 0.001 for both).
The analysis found that testing positive for any E antibodies produced an 80% reduction in mortality risk (hazard ratio [HR], 0.2; 95% confidence interval [CI], 0.1-0.4) and disease progression. In particular, patients with E1, E6, and NE2 antibodies had significant overall and progression-free survival rates.
"When we look at the entire cohort, we expect that more than 80% are HPV-positive, thus driving the association between HPV antibody positivity and improved survival," lead study author Kristina Dahlstrom, PhD, an instructor in the head and neck surgery department at MD Anderson, told DrBicuspid.com.
The investigation found that E antibody positivity served as a better predictor for overall and progression-free survival (p < 0.001 for both) than for HPV positivity (overall survival, p = 0.031; progression-free survival, p = 0.016). However, both factors conferred an 80% reduction in the risk for death and a strong association with improved progression-free survival.
Misclassified patients
The study had several limitations, which could limit the ability to isolate the effects of individual antibodies, according to the study authors. First, a large proportion of patients whose tumors were negative for HPV16 DNA were positive for at least one E antibody (13 of 18, 72.2%). Conversely, a subset of patients whose tumors were positive for HPV16 DNA were negative for all E antibodies (10 of 96, 10.4%), but these patients may have been misclassified. And although the study included 209 patients, researchers had HPV16 status for only 114, limiting the analysis to 96 patients with HPV16-positive tumors.
Dr. Sturgis said that his colleagues, Bonnie Glisson, MD, and Erminia Massarelli, MD, PhD, are overseeing a clinical trial at MD Anderson for recurrent and metastatic HPV-related cancers. That trial uses a vaccine for E6 and E7 antibodies in combination that targets PD1 proteins, he explained.
"Our results show that HPV16 antibody status, in particular E antibody status, is a strong predictor of survival among patients with HPV-positive oropharyngeal carcinoma," the study authors concluded. "Specific antibody status has the potential to be a useful prognostic indicator that may identify subsets of patients diagnosed with HPV16-positive tumors who may benefit from altered monitoring and/or treatments. In addition, the suggestion that immune response to HPV16 antigens is important to cancer outcomes suggests the potential of augmenting immune responses to improve treatment of patients with HPV-driven oropharyngeal carcinoma."