A 3D facial scan can help dentists and doctors screen patients for undiagnosed obstructive sleep apnea (OSA), according to the findings of a study published on April 15 in the Journal of Clinical Sleep Medicine.
OSA is a common yet potentially deadly condition -- and one where the majority of cases go unidentified. A quick and painless series of photographs may identify patients who need to be tested better than other screening modalities, such as questionnaires.
"OSA is a huge public health problem, and despite effective treatments being available, many with OSA are currently undiagnosed," stated lead study author Peter Eastwood, PhD, from the Centre for Sleep Science at the University of Western Australia, in a press release. "Therefore, simple, accurate screening tools are needed to predict those who have OSA."
Researchers know that the width of the middle and lower face correlates with OSA severity, and they wondered whether 3D photographs could be used to help determine which patients might have OSA.
For the study, the authors recruited 50 people without obstructive sleep apnea and 300 people with mild, moderate, or severe OSA. All participants had 180° 3D face scans with a 3dMD craniofacial scanner system.
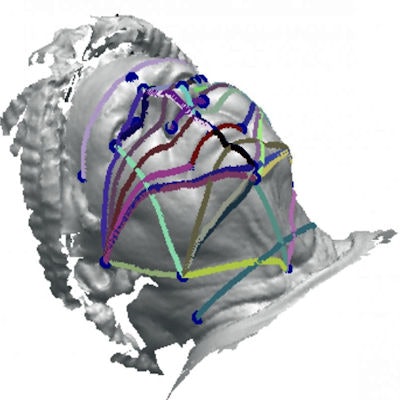
 Linear and geodesic measurements from 3D photographs could predict OSA likelihood. Image courtesy of the Journal of Clinical Sleep Medicine.
Linear and geodesic measurements from 3D photographs could predict OSA likelihood. Image courtesy of the Journal of Clinical Sleep Medicine.The authors selected 25 pairs of landmarks from the facial scans and calculated the linear and geodesic (curved) dimensions between them. Both measurements showed great aptitude for predicting OSA when combined with body mass index (BMI) and neck circumference data.
The geodesic measurements alone had an accuracy of 89%, which was significantly higher than the 86% accuracy of linear measurements alone. When the researchers combined the two measurements, the accuracy rate rose to 91%.
Participants with OSA had significantly different face depths, widths, mandibular dimensions, and neck widths than their peers without OSA. The dimensions were most drastic for the mandibular width angle, lower facial width angle, and maxillary-mandibular relationship angle.
The dimensions also differed for people with varying degrees of obstructive sleep apnea severity. Specifically, upper and lower face depth, total and upper face height, lateral face height, face width, mandible width, and neck width differed between people with mild, moderate, and severe sleep apnea.
It is important to note that the sensitivity, specificity, and accuracy of the model decreased with higher sleep apnea cutoffs (e.g., 10 events per hour instead of five events per hour). The test also had a specificity of only 76%, suggesting it may be better as a screening tool rather than a diagnostic.
"The method described in this study demonstrates the potential for 3D facial photographs to provide a rapid, simple, objective, and accurate method to identify individuals at high risk of OSA," the authors wrote. "Although it was developed using an expensive, high-resolution, research quality craniofacial scanner system, it might be possible to embed such a method into existing, cheap, off-the-shelf 3D photography systems."