Diode laser-assisted oral surgery offers many advantages when removing benign, premalignant, or malignant lesions or venous malformations from patients' oral cavities, according to a case report published on July 20 in the Cureus Journal of Medical Science.
Benefits include decreasing the amount of local anesthesia required, improving the speed and precision of procedures, and avoiding the need for stitches, the authors wrote. Their report showcases the use of diode laser-assisted oral surgery in a series of patients.
"The achievable clinical advantages are essentially related to the intrinsic properties of the diode laser wavelength that, if correctly used, may simplify all procedures of minor and major oral surgery," wrote the group, led by Domenico De Falco from the faculty of dentistry at the University of Bari Aldo Moro in Bari, Italy.
Diode lasers use continuous-wave and pulsed-wave modes to perform dental procedures. They are used most often to remove proliferating lesions and to photocoagulate vascular malformations in the oral cavity. These tools result in no intraoperative bleeding, make it easier to treat conditions located in hard-to-reach areas, and reduce postoperative edema and pain, according to the authors.
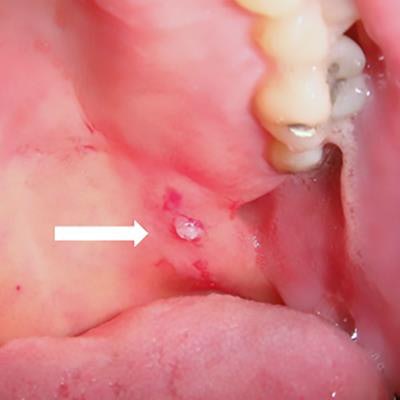
A 45-year-old woman
A painless, small nodular lesion developed within a white lesion located in a patient's soft palate. The lesion, which was there for eight months, was removed via laser due to its anatomic site and the difficult surgical approach. The patient was given local anesthesia and light conscious sedation. The surgery was easy, she didn't bleed, and she didn't experience any postoperative complications. The thermal cut didn't alter the specimen, and it was diagnosed as a leukoplakia-associated mucocele without signs of dysplasia, likely related to her smoking habit. She healed in 10 days, and there was no recurrence.
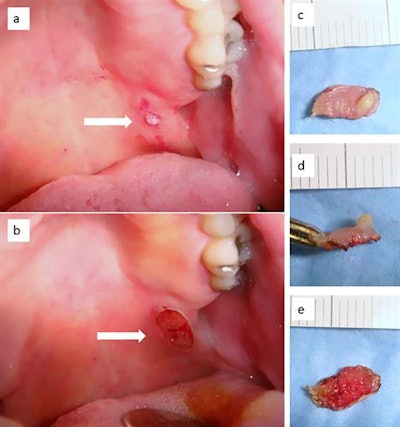 A: Small nodular lesion within a larger white lesion of the patient's posterior soft palate. B. After the lesion was removed by a diode laser. C-E: Various images of the surgical specimen, which is well conserved and shows no sign of carbonization, which can affect histological readability. All images courtesy of DeFalco et al. Licensed under CC BY-NC 4.0.
A: Small nodular lesion within a larger white lesion of the patient's posterior soft palate. B. After the lesion was removed by a diode laser. C-E: Various images of the surgical specimen, which is well conserved and shows no sign of carbonization, which can affect histological readability. All images courtesy of DeFalco et al. Licensed under CC BY-NC 4.0.A 47-year-old man
The patient had an immobile, painless nodular lesion in the paramedian position at the base of the uvula of his soft palate for six months. A diode laser was used due to the location and the suspicion that it may have been a proliferating viral lesion. The patient underwent local anesthesia, and the lesion was excised. The surgery was quick and resulted in no bleeding, complications, or recurrence. It was diagnosed as a viral papilloma, according to the authors.
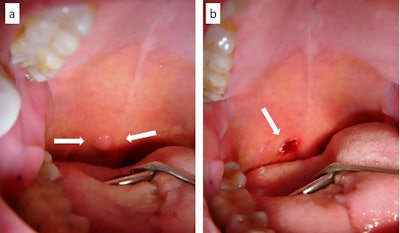 A: A viral papilloma of the posterior soft palate. B: The site after the papilloma was removed with a diode laser.
A: A viral papilloma of the posterior soft palate. B: The site after the papilloma was removed with a diode laser.A 58-year-old man
A 58-year-old smoker who wore implant-retained prostheses and experienced biting trauma for quite some time exhibited a dishomogeneous leukoplakia in his left cheek. The patient underwent light conscious sedation, and a diode laser was used to remove the entire lesion due to the dimensions and the impossibility of performing an incisional biopsy. No bleeding occurred during the procedure, and no stitches were required. He was diagnosed with frictional keratosis and healed in 18 days.
 A: A large dishomogeneous leukoplakia patch on the cheek of a smoker. B: Lugol's solution provides a more defined view of the patch, which was diagnosed as frictional keratosis. C: A diode laser was used to excise the patch. D and E: The surgical sample. F: Eight days after surgery. G: Complete healing after 18 days.
A: A large dishomogeneous leukoplakia patch on the cheek of a smoker. B: Lugol's solution provides a more defined view of the patch, which was diagnosed as frictional keratosis. C: A diode laser was used to excise the patch. D and E: The surgical sample. F: Eight days after surgery. G: Complete healing after 18 days.A 64-year-old man
A 64-year-old man with occasional biting trauma had a blue-violet, immobile, painless, and nonbleeding lesion of the cheek for a year. He was prescribed the blood thinner warfarin for chronic atrial fibrillation. An ultrasound scan confirmed his diagnosis of venous malformation. The man underwent transmucosal photocoagulation by diode laser without suspending his warfarin treatment. He received a small amount of local anesthesia, and a laser was used to photocoagulate the lesion directly. Treatment ended when the lesion's color changed to grayish-white. It healed in 14 days without recurrence.
 A: A blue-violet appearance of a venous malformation of the cheek mucosa. B: The diode laser confirmed transmucosal photocoagulation when the malformation changed color to grayish-white. C: The irradiated area healed in 14 days.
A: A blue-violet appearance of a venous malformation of the cheek mucosa. B: The diode laser confirmed transmucosal photocoagulation when the malformation changed color to grayish-white. C: The irradiated area healed in 14 days.A 66-year-old woman
The patient had proliferative verrucous leukoplakia, tested positive for the hepatitis C virus, and exhibited a potentially malignant lesion of the soft palate. She had multiple nodular lesions within a dishomogeneous leukoplakia. Considering the difficulties in treating the lesion with conventional scalpel surgery and the potential increase in bleeding due to liver disease, an excision was performed via diode laser while she was under general anesthesia. No intraoperative or postoperative bleeding occurred, and she was completed healed by secondary intention within 22 days. Her final diagnosis was early oral squamous cell carcinoma due to the malignant transformation of proliferative verrucous leukoplakia.
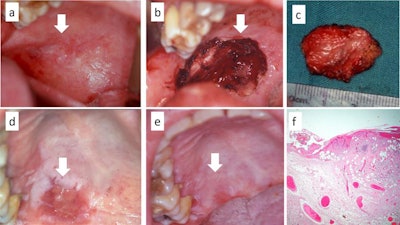 A: A malignant transformation of proliferative verrucous leukoplakia of the soft palate. B and C: The entire lesion was excised with the laser without direct suture of the margins. D: A view of the partially healed lesion. E: Complete healing of the palate after 22 days. F: The histological exam shows foci of early oral squamous cell carcinoma.
A: A malignant transformation of proliferative verrucous leukoplakia of the soft palate. B and C: The entire lesion was excised with the laser without direct suture of the margins. D: A view of the partially healed lesion. E: Complete healing of the palate after 22 days. F: The histological exam shows foci of early oral squamous cell carcinoma.Many uses
Diode lasers have numerous clinical applications in dentistry, and clinicians should take advantage of all they have to offer patients.
"With [diode laser] use, the need for general anesthesia certainly decreases for the treatment of oral lesions with wide dimensions or those occurring in uncomfortable anatomical sites or uncooperative patients/children, and more frequently, may be replaced by easily manageable conscious sedation," the authors wrote.



















