Clinicians have successfully used antibiotics and steroids, instead of an aerosol-generating procedure, to treat a COVID-19-positive man's peritonsillar abscess. Details were published on September 7 in BMJ Case Reports.
This is the first reported case of a patient having a peritonsillar abscess and COVID-19, according to the authors. Clinicians need to be aware that these conditions can occur simultaneously, and they should, therefore, avoid using high-risk procedures such as transoral drainage to treat abscesses. Instead, they should consider treatments that limit the risk of infection, they wrote.
"Peritonsillar abscess may be managed with high-dose intravenous antibiotics and steroid therapy without undue risk to healthcare workers or compromising patient outcome," wrote the group, led by Anders Williams Sideris, MD, from Wollongong Hospital in New South Wales, Australia.
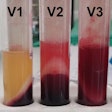
 Computed tomography scan of a peritonsillar abscess in a 21-year-old man. All images courtesy of BMJ Case Reports.
Computed tomography scan of a peritonsillar abscess in a 21-year-old man. All images courtesy of BMJ Case Reports.Simple procedure, complicated times
A peritonsillar abscess is a bacterial infection, often arising as a complication of tonsillitis or strep throat. Typically, the infection involves a pus-filled pocket that forms near the tonsils. For decades, the standard treatment for abscesses has been to aspirate them with needles or drain them.
The COVID-19 pandemic has made transoral drainage a high-risk procedure due to potential aerosolization. Therefore, in the current case, healthcare workers needed to manage the abscess with a more conservative approach.
A 21-year-old man
After experiencing a sore throat, fever, progressive painful swallowing, and voice changes for five days, the man visited a local hospital and was admitted. He had no other symptoms associated with SARS-CoV-2, but two tests confirmed he was positive. Seven weeks earlier, the man had returned to Australia following a six-month stay in Canada. He underwent mandatory pandemic home quarantine for 14 days upon his return.
Clinicians discovered during an oral exam that he had peritonsillar swelling on the right side, red patches surrounding it, and uvula deviation, and his jaw range of motion was limited. These symptoms were consistent with a peritonsillar abscess, according to the authors.
A computed tomography (CT) scan confirmed the abscess. The man was admitted to the hospital and given high-dose intravenous antibiotics and steroid therapy to manage the abscess and to limit healthcare workers' exposure to SARS-CoV-2, they wrote.
After treatment
Two days after his discharge from the hospital -- 14 days from the start of his symptoms -- the patient tested negative for the novel coronavirus. The peritonsillar abscess had been treated successfully, his oral cavity was normal, and he could eat and drink without difficulty four days after his discharge. Four days later, a CT scan confirmed the complete resolution of the abscess and the antibiotics were stopped, according to the authors.
 CT results after treatment of the abscess.
CT results after treatment of the abscess.The only limitation to the medication approach was that it required the patient to spend several days in the hospital. Having an abscess drained is an outpatient procedure, the group noted.
 The man's mouth during an oropharyngeal examination after treatment.
The man's mouth during an oropharyngeal examination after treatment.Heed with caution
Most importantly, this case highlights the importance of considering other treatments during a worldwide pandemic, even in areas that reported no new cases of COVID-19. When the 21-year-old visited the hospital, there had been no new reported cases in the area for five weeks. Australia reported only 12 new cases one day prior to this man's diagnosis, the authors wrote.
"This case should remind physicians to maintain a high degree of suspicion in areas of low prevalence of COVID-19, especially when assessing patients with symptoms of upper respiratory tract infection and presentations such as peritonsillar abscess," they concluded.