After years of treatment, lab results revealed that a 57-year-old woman did not have peri-implantitis but the rare inflammatory disease intraosseous sarcoidosis, according to a case report published on November 29 in the Journal of Oral and Maxillofacial Surgery.
This is believed to be the first case reported in an English publication. Clinicians should consider sarcoidosis as a possible diagnosis for patients with lasting, nonhealing bony lesions in the maxillofacial region who have not been exposed to osteoclast inhibitory therapy or radiation. Diagnosis should be confirmed with lab analysis of bone and surrounding tissue, the authors wrote.
"Our patient had an unusual presentation of intraosseous sarcoidosis mimicking peri-implantitis," wrote the group, led by Dr. Jay Buckey Jr. from the Geisel School of Medicine at Dartmouth College.
Delayed healing
Peri-implantitis causes inflammation in the peri-implant connective tissue and progressive loss of supporting bone surrounding the dental implant. Though peri-implantitis is predominantly a local condition, there are systemic issues that can prevent healing.
In most cases, when healing is delayed after an implant fixture is removed and the bone in the maxillofacial area is exposed, it is due to conditions such as medicine-related osteonecrosis of the jaw. Sometimes, systemic conditions, including chronic steroid use or uncontrolled diabetes, can cause prolonged infections. However, other medical conditions, such as sarcoidosis, also can lead to a similar presentation, according to the authors.
In 1869, sarcoidosis was first described as a skin condition. Sarcoidosis is characterized by widespread T-cell dysfunction and increased B-cell activity that results in areas of inflammation that may lead to fibrosis and calcium dysregulation.
Since then, the medical profession's understanding of sarcoidosis has evolved. In addition to skin conditions, sarcoidosis can affect other parts of the body, including the lungs. Also, there is bone sarcoidosis, which is very rare, but when it occurs, it presents in the small bones of the hands, feet, spine, and pelvis.
Sarcoidosis is extremely rare in the maxillofacial bony region. Only 26 other cases have been reported in this region, the authors wrote.
Years of problems before a diagnosis
In 2013, the 57-year-old woman had two teeth extracted, and the sockets were preserved in preparation for future implant placement. At the time, the woman reported not using antiresorptive or antiangiogenic medications that could cause medication-related osteonecrosis of the jaw. In 2014, two dental implants were placed. At a three-month checkup, the woman was given implant-supported crowns.
In December 2016, the woman began experiencing bleeding and swelling near the implants, suggesting peri-implantitis. She was treated with antibiotics for 10 days and told to improve dental hygiene and use chlorhexidine rinses. This moderately improved her symptoms, the authors wrote.
In March 2017, the woman's symptoms returned, and pus was draining from the peri-implant sulcular tissue. Again, clinicians prescribed her antibiotics and rinses. The woman also underwent debridement to remove granulation tissue near the implant collar region.
Despite these dental interventions, her symptoms, including pus drainage, returned. Therefore, surgeons opted to remove the implant-supported crowns, explant the implant fixtures, augment the site with a bone graft, cover it, and obtain primary mucosal closure. Also, a prolonged course of antibiotics was prescribed.
A month later, clinicians could see pus draining, wound breakdown, and exposed bone. Debridement was performed, and the section was cultured. Though the sample was positive for microaerophilic Streptococci and Acinetobacter, the woman declined to have the bone submitted for pathological analysis and a review by infectious disease doctors. She was prescribed a stronger antibiotic.
Her mouth began to heal slowly over several months, but exposed bone at the crest of the ridge could be seen. The patient underwent a panoramic x-ray, which revealed hyperdensity above her inferior alveolar nerve canal with densely calcified hard crystal material. She was treated for chronic low-grade osteomyelitis.
In June 2018, the woman's pain returned, and she sought a second opinion. She was diagnosed with chronic refractory osteomyelitis and was treated with hyperbaric oxygen. During the oxygen treatments, she reported experiencing chest tightness, the authors wrote.
In November 2018, after 19 hyperbaric oxygen treatments, the woman reported experiencing wheezing, chest tightness, and trouble breathing. The woman was hesitant to seek other treatments or consultations and continued with local wound care and observation.
Since her lung symptoms didn't improve, she underwent a computed tomography (CT) scan in March 2019. The scan showed mediastinal lymphadenopathy and parenchymal lung opacities. She had decreased lung capacity and was started on steroids and an inhaler.
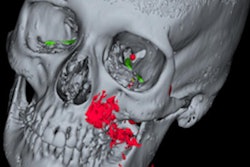
In August 2019, a CT scan of her jaw was taken, which showed 2.5 cm of erosive osseous defects suggestive of osteomyelitis. An infectious disease specialist recommended a biopsy of her mandible.
In September 2019, the woman underwent debridement and biopsy. The results showed evidence of nonnecrotizing granulomatous inflammation, and she was prescribed eight weeks of intravenous antibiotics. Also, she underwent a mandibular and thoracic lymph node biopsy, which demonstrated results consistent with sarcoidosis.
"Although previously thought to be a jaw infection, the biopsy findings of the jaw and clinical picture excluded other etiologies, and the patient's non-healing bony lesion of the mandible was understood to be bone sarcoidosis with her implants serving as a nidus for sarcoid granuloma formation," the authors wrote.
Subsequently, she was prescribed steroids and antibiotics, but the patient also had bone loss around teeth located near the implants. Those two teeth were pulled, and debridement was performed. She healed without any other complications.
In early 2021, the woman experienced significant improvement taking steroids, an immunosuppressive drug, and folic acid.
"Intraosseous sarcoidosis should be considered on the differential for patients experiencing extraoral manifestations of sarcoidosis, a preexisting condition, or in the case of our patient, persistent bony problems despite adequate surgical and medical intervention," Buckey and colleagues wrote.