A 69-year-old woman developed black hairy tongue (BHT) after taking an antibiotic commonly prescribed to treat bacterial infections, according to a recent case report published in the American Journal of Case Reports.
Several types of antibiotics, including penicillin and cephalosporin, are linked to this unusual benign condition, which presents as a superficial black, hairy, carpetlike lingual growth. However, this incident is believed to be the first reported case of moxifloxacin-induced BHT, the authors wrote.
"Clinicians should be aware of agents or lifestyles that may cause BHT, and it is essential to counsel on the possibility of developing BHT before starting treatment to avoid patient anxiety or premature treatment cessation," wrote the authors, led by Dr. Mikiro Kato of the department of infectious diseases at the University of Tsukuba Hospital in Japan (Am J Case Rep, April 25, 2022, Vol. 23:e936235).
69-year-old woman with a discolored tongue
After developing a brown discoloration on her tongue, the patient visited the clinic. She was taking an oral steroid daily for her mixed connective tissue disease, and she also had high blood pressure, high cholesterol, diabetes, and osteoporosis, according to the report.
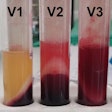
 A 69-year-old woman developed a brown discoloration with carpetlike elongated filiform papillae after taking moxifloxacin. Image courtesy of Kato et al. Licensed by CC BY 4.0.
A 69-year-old woman developed a brown discoloration with carpetlike elongated filiform papillae after taking moxifloxacin. Image courtesy of Kato et al. Licensed by CC BY 4.0.Approximately three months prior to her visit to the clinic, the woman underwent debridement and reconstructive surgery for right index and middle finger flexor tenosynovitis. The procedure was complicated by osteomyelitis caused by Mycobacterium chelonae, the authors of the case report wrote.
For six weeks, she was treated with intravenous tobramycin and imipenem and oral clarithromycin. Then, her antibiotic regimen was switched to oral moxifloxacin and clarithromycin.
Within 10 days after the switch, the woman noticed changes in the color of her tongue. When she went to the clinic, she had no fever or any other symptoms. She denied any medication changes, use of herbal or Chinese medicines, smoking, or alcohol. Also, the patient reported she had not used any tongue scrapers, cleaners, or mouthwashes, according to the report.
Further examination revealed that her vital signs were normal. An oral exam showed that her mucosa was dry, and there was brown discoloration on the dorsum of her tongue, with carpetlike elongated filiform lingual papillae. However, the woman didn't have caries, bad breath, bleeding, discharge, or exudates.
Due to her not having significant symptoms, a tongue swab culture wasn't performed, they wrote. The clinician gave her a tentative diagnosis of stained tongue due to food or BHT from antibiotics. For two weeks, the woman was observed with daily oral hygiene and tongue scraping. However, her discoloration and elongated filiform lingual papillae didn't improve.
The patient did not want to continue taking the antibiotics. Due to the lower susceptibility of moxifloxacin for isolated Mycobacterium chelonae, the use of that antibiotic was discontinued, and she continued to take clarithromycin. Within two days of her discontinuing the moxifloxacin, her tongue improved to normal, the authors wrote.
Rare condition with an unclear origin
The prevalence of BHT ranges from 0.6% to 11.3% depending on factors such as age, sex, and ethnicity. The etiology of BHT remains unclear, although it is believed to be likely multifactorial.
Possible contributing extrinsic factors can include heavy use of tobacco or alcohol, and possible intrinsic factors can include poor oral hygiene, HIV, or trigeminal neuralgia. Additionally, dry mouth can be a risk factor, according to the report.
To avoid patient anxiety and unexpected treatment changes, patients should be counseled about the possible development of BHT associated with certain medications and lifestyle factors, the authors wrote.
"Clinicians should be vigilant against agents and lifestyles that can precipitate BHT, especially moxifloxacin," Suzuki and colleagues wrote.