A 7-year-old boy with congenital heart disease developed multiple brain abscesses caused by an infection from apical periodontitis in his baby teeth, according to a case report published on June 28 in BMC Oral Health.
The abscesses immediately became smaller, and his neurological symptoms disappeared after the extractions. This case highlights the importance of knowing that many diseases originating from dental infections can be treated with appropriate therapies, the authors wrote.
"In the current case, removal of the deciduous teeth, which were suspected to have been the source of the infection, seemed to be effective even with serious brain abscess considering that the patient's symptoms improved after the extraction," wrote the authors, led by Dr. Takashi Kikuiri, Department of Pediatric Dentistry, Nihon University School of Dentistry in Tokyo.
7-year-old boy with fever, headaches
On September 8, 2020, a boy with complete atrioventricular septal defect, pulmonary atresia, major aortopulmonary collateral artery, and total anomalous pulmonary venous connection with pulmonary vein stenosis went to a hospital due to a fever and headaches.
He was diagnosed with multiple brain abscesses and prescribed multiple antibiotics. He also underwent blood tests, which came back positive for Streptococcus intermedius and Staphylococcus aureus. After two weeks, the boy's symptoms of fever and headache improved, they wrote, but by September 26, his neurological symptoms reappeared.
Magnetic resonance imaging (MRI) revealed exacerbation of his brain abscess and circumferential swelling. The patient was transferred to another hospital, and placed on the same course of antibiotic treatment, the authors wrote.
At the new hospital, the boy underwent a whole-body MRI to identify the fungus and source of infection. The MRI revealed several lesions in his frontal lobe, basal ganglia, thalamus, and bilateral temporal lobes. Due to these findings, clinicians suspected a blood-based infection due to multiple brain abscesses, they wrote.
An echocardiogram showed no vegetation in the heart. Clinicians reread the positron emission tomography (PET) and computed tomography (CT) images taken at the first hospital and saw no obvious source of infection in the system or otolaryngological areas. New blood cultures taken tested negative.
To gain further insight into the source of infection, the boy was referred on September 29 to the hospital's pediatric dentistry department. Intraoral images showed several unfavorable fillings in his baby teeth, and panoramic x-rays showed periapical transmission and root resorption in his upper and lower deciduous molars, the authors wrote.
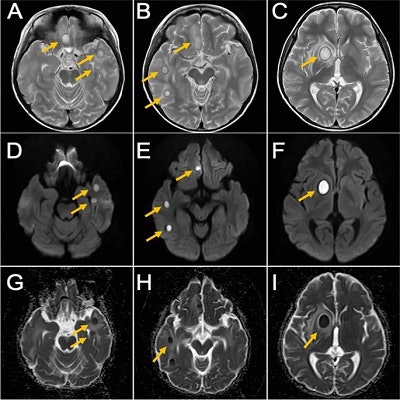
 MRI of the boy’s brain obtained on September 26, 2020. T2-weighted image (A, B, and C), diffusion-weighted image (D, E, and F), ADC map (G, H, and I). Yellow arrows indicate brain abscesses. There were multiple nodular lesions showing ring-like hyperintensity in T2-weighted images and internal hyperintensity and decreased ADC in diffusion-weighted images.
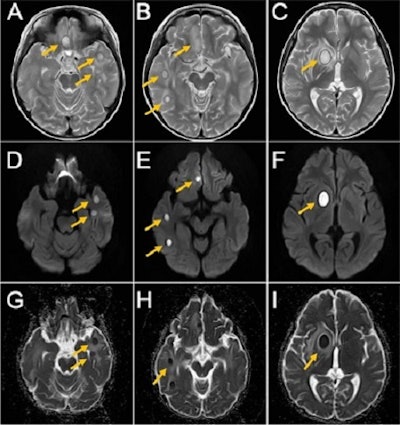
MRI of the boy’s brain obtained on September 26, 2020. T2-weighted image (A, B, and C), diffusion-weighted image (D, E, and F), ADC map (G, H, and I). Yellow arrows indicate brain abscesses. There were multiple nodular lesions showing ring-like hyperintensity in T2-weighted images and internal hyperintensity and decreased ADC in diffusion-weighted images.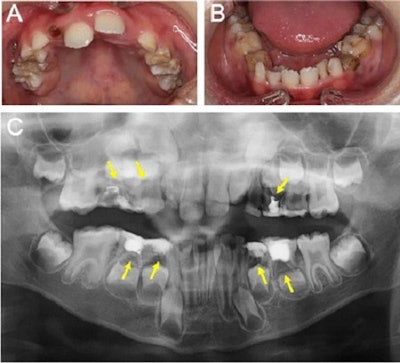 Clinical and x-ray findings of the boy at the initial visit. Intraoral photograph (A and B) and panoramic x-ray (C) of the boy at his initial visit. Yellow arrows indicate apical periodontitis.
Clinical and x-ray findings of the boy at the initial visit. Intraoral photograph (A and B) and panoramic x-ray (C) of the boy at his initial visit. Yellow arrows indicate apical periodontitis.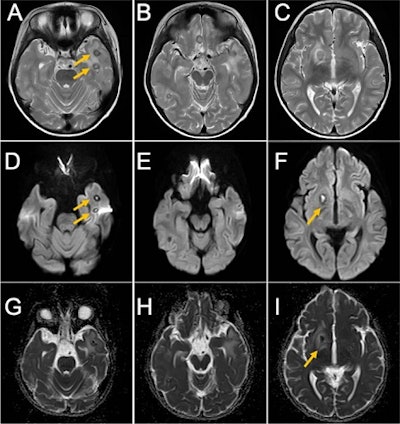 MRI obtained of the boy's brain obtained on November 11, 2020. T2-weighted image (A, B, and C), diffusion-weighted image (D, E, and F), ADC map (G, H, and I). Yellow arrows indicate brain abscesses. Images courtesy of Kikuiri et al. Licensed by CC BY 4.0.
MRI obtained of the boy's brain obtained on November 11, 2020. T2-weighted image (A, B, and C), diffusion-weighted image (D, E, and F), ADC map (G, H, and I). Yellow arrows indicate brain abscesses. Images courtesy of Kikuiri et al. Licensed by CC BY 4.0.Clinicians believed that the blood-based brain abscess relied on the infection of the primary lesion. Since the exam revealed no potential causative factor other than dental infection, apical periodontitis of baby teeth was considered the source of multiple brain abscesses.
Know the risks
In this case, the patient's baby teeth were extracted under local anesthesia in October. Immediately after the procedure, the boy's neurological symptoms disappeared. By early November, his latest administration of the antimicrobial agent was completed, and his general condition had improved considerably.
One month after his teeth were pulled, the boy underwent an MRI that revealed that the brain abscess was still there but noticeably reduced. On November 17, he was discharged from the hospital.
In those with cyanotic congenital heart diseases with right to left shunt, like the boy in this case, deoxygenated blood may enter systemic circulation directly, putting them at a greater risk of brain abscess development. Though mandibular osteomyelitis originating from dental infections is common, inappropriate treatment can lead to severe complications that can be life threatening, Kikuiri and colleagues wrote.
"Patients with severe cyanotic congenital heart disease may develop serious brain abscesses, indicating the importance of continued administration of antibiotics during dental treatment, appropriate follow-up after dental treatment, and employment of proper measures when signs of foci formation are observed," they wrote.