DrBicuspid.com is pleased to present the next column from two lawyers who spend every day defending dentists in litigation and before the licensing board. The purpose of this column is to offer our readers a fresh perspective on common practice and risk management issues from attorneys who litigate these issues in the real world.
The patient, a 35-year-old stockbroker and father of two teenagers, presented to his general dentist with episodic pain in the upper left quadrant of his mouth. He had been a patient for some 10 years, coming in occasionally for examinations and cleanings, but generally presented when he had a problem, just as he did in this situation.
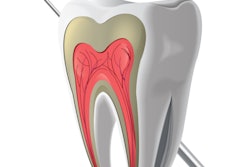
In the past, the dentist had performed root canal therapy (RCT) on two nonvital teeth, and on both occasions he prescribed amoxicillin as part of the treatment protocol. The dentist took a full series of x-rays and performed a thorough examination. The upper left first molar, #14, was mildly responsive to various applied stimuli, vitality testing was equivocal, and it had what appeared to be a small radiolucency at the apex of the mesiobuccal root.

As he had done for the previous root canals, the dentist prescribed antibiotics, because the patient needed to schedule time out of work in advance and the dentist wanted to avoid a flare-up. This time, he prescribed clindamycin, 300 mg, QID, for one week, and scheduled the root canal therapy appointment for three days after the initial visit, which would be in the middle of the clindamycin course.
The dentist's decision to employ clindamycin instead of amoxicillin was based on his having attended study groups at which the issue of antibiotic choice was discussed. He learned from several colleagues, including an endodontist, that they were having better success with clindamycin in keeping nonvital teeth quiet. The dentist advised the patient that gastrointestinal (GI) symptoms may arise from the medication and asked him to cease the antibiotic and call if that did happen.
The planned root canal therapy visit was uneventful: A necrotic pulp was found; a pulpectomy was done; the antibiotics -- which had caused no GI symptoms to date -- were to be continued (with a refill prescription given to carry the patient past the RCT completion visit); and an appointment given to finish the root canal therapy.
The next day, a Saturday, the patient awoke with severe intestinal pain and diarrhea, and he called the dentist's cellphone, which was made available to all patients. The dentist, on hearing the symptoms, told the patient that he need not worry because this was a common side effect, and called in a prescription for the antidiarrheal Lomotil (atropine and diphenoxylate), advising him to take it until the next visit on Thursday. The patient filled the prescription and took it as prescribed.
On Tuesday, the patient's wife, also a patient of the dentist, called the office and said that her husband had been taken to the hospital by ambulance with unbearable abdominal pain. Despite attempts to resolve the situation, the patient died on Wednesday night. The autopsy report cited the cause of death as complications of toxic megacolon, resulting from antibiotic-induced Clostridium difficile-related pseudomembranous colitis and decreased motility of the colon.
Legal stance
The patient's wife filed suit. Her attorneys claimed dental malpractice against the dentist, now our client, asserting the following:
- The dentist improperly gave an antibiotic in the absence of clear signs of infection.
- The dentist made an improper antibiotic choice by prescribing clindamycin instead of amoxicillin or other penicillin-type of antibiotic.
- The dentist should not have prescribed lomotil, especially over the phone.
- The dentist should have involved a physician in the care of the patient once the patient experienced GI distress.
The damages sought on behalf of the husband were the pain and suffering in the period of time leading up to his death, as well as his lost high six-figure income for his anticipated working life of some 30 years; the wife sought money for her own loss of consortium.
We retained as experts a general dentist who regularly does root canal therapy and a physician specializing in infectious diseases.
Issues raised
- Prescribing of an antibiotic: While divergent views exist within dentistry as to when to prescribe antibiotics, our client believed that he was justified in doing so because he had success in the past doing the same and, most important, because the patient had radiographic periapical pathology. Our dental expert was able to support the dentist's action in this regard.
- Antibiotic choice: Clindamycin has good coverage for the bacteria generally associated with dental infections. An argument can be made that its coverage is superior to amoxicillin; so the choice comes down to whether the potential side effects of clindamycin outweigh its therapeutic benefits when compared with amoxicillin or even another penicillin derivative. As it turns out, our infectious-diseases expert is of the view that both types of medications are almost equally likely to cause colitis and its associated complications. Based on our infectious-disease expert's view and supporting peer-reviewed literature, we felt confident defending this aspect of care.
- The use of Lomotil and doing so without physician referral: From a purely legal standpoint, a dentist in New York may properly prescribe Lomotil, but whether that should be done, from a risk-management perspective, is a separate question altogether, and it is a subject of debate that we do not comment on here. Lomotil's mechanism of action is to slow down the intestinal removal of its contents, so that intestinal contents which are best ridded quickly are left inside. It is for this reason that contraindications for the use of lomotil include pseudomembranous colitis and enterotoxin-producing bacteria; in simple terms, it is properly avoided with antibiotic-induced diarrhea. The fact that the dentist's decision to prescribe Lomotil was made based on a phone conversation did not have a practical difference as compared with doing so at a visit, but it does not look good to a jury.
Result
Issues related to the Lomotil were problematic, and neither of our experts was able to fully defend this aspect of the case. The potential downside of allowing a jury to award huge sums of money, especially for 30 years of lost earnings, led the dentist to consent to settle the case. However, in the face of an exorbitant settlement demand, we had no alternative but to commence the trial.
The case settled on trial for a small fraction of the starting demand and for a number well below the dentist's policy limits.
Practice tips
- Prescription of an antibiotic: Antibiotics are serious medications with serious potential side effects, and they must be respected for exactly that. A properly thought out and justifiable determination of the need for antibiotics needs to be done each and every time.
- Antibiotic choice: There are almost always choices among antibiotics and, in fact, among all types of drugs prescribed in dental practice. When one drug is chosen over another, there should be a solid scientific basis for doing so; while study clubs offer an excellent forum for the exchange of ideas, and what is learned by attending is valuable, they are not scientific studies. It is not uncommon that a drug is chosen that has serious known side effects, but that does not necessarily exclude its use if there is an in-depth thought process before it is chosen.
- The use of Lomotil and doing so without physician referral: In dental practice, there are clearly a number of medications that are frequently used and some rarely used. It is always important to stay current on medical issues and certainly be fully familiar with the drugs you use regularly, but when you prescribe a drug that you have rarely or never before used, take some time and become familiar with it. If you are unfamiliar with any situation, tell patients that you want to consult with another doctor or that you want to do a bit of research, and you will get back to them.
- Follow-up: When patients call with complications, whether from actual treatment or from medication side effects, it generally means that something is going wrong and it may not resolve on its own. Of course, there are always going to be patients who unnecessarily complain, so it is critical to the care of the patient and critical to potential liability to accept patient complaints as legitimate and stay in close touch with them until the problem resolves or the patient is referred. Keeping tight control over complications is part of what dental practice is all about, and it surely makes lawsuits less likely if things go wrong.
William S. Spiegel, Esq., is a partner at the law firm Spiegel Leffler in New York City. He is a former assistant corporation counsel to the City of New York -- Medical Malpractice Division.
Marc R. Leffler, DDS, Esq., is also a partner at Spiegel Leffler. He received his dental degree from Columbia University, completed a residency in oral and maxillofacial surgery at New York University, and is a diplomate of the American Board of Oral and Maxillofacial Surgery.
Disclaimer: Nothing contained in this column is intended as legal advice. Our practice is focused in the state of New York, and there are variations in rules of practice, evidence, and procedure among the states. This column scratches the surface on many legal issues that could call for a chapter unto themselves.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.