Before bandaging a wound, you apply an antibiotic ointment. Before probing a tooth, you sterilize your explorer. So should you also disinfect a tooth before placing the restoration?
Dentistry has gone back and forth on this question, wrote Rella Christensen, R.D.H., Ph.D., in the Gordon J. Christensen Clinicians Report (November 2009, Vol. 2:11, pp. 1-2), adding that in recent years most dentists have not worried much about disinfecting preparations.
"If I were a dentist, I would use a fast, broad-spectrum-kill disinfectant before I applied my restorative materials," she told DrBicuspid.com.
— Rella Christensen, R.D.H., Ph.D.
In a study of 28 live patients, Christensen and her colleagues Brad Ploeger and Theresa Rich, M.S., found that water-cooled cutting, rinsing, drying, and acid etching, with or without rubber dam isolation, didn't kill the organisms present on the tooth surface.
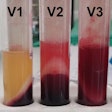
So they advocate treating the preparations with a solution of 5% glutaraldehyde and 35% hydroxyethyl methacrylate (HEMA). This solution, which was marketed first as a part of a dental adhesive system and then as a desensitizer, is also a powerful disinfectant, though not FDA-cleared for this purpose, said Christensen, who has studied glutaraldehyde since the mid-1970s. The researchers found that the solution provided a good disinfection of the preparation.
This compound is proved to be compatible with common resin dental materials, kills a broad spectrum of microorganisms, and has a good wetting action on cut tooth, Christensen said. And unlike some of the more commonly used oral disinfectants, including chlorhexidine and sodium hypochlorite, 5% glutaraldehyde is not easily deactivated by biological proteins such as those present in cut dentin, blood, saliva, and plaque, she said.
Christensen added that Technologies in Restoratives and Caries (TRAC) Research, where she is section leader, is still studying whether this treatment makes a difference in the patient's health. "We don't have the follow-up data yet, and we probably won't for a year," she said.
Entombing the microbes
Asked to comment, Douglas Young, D.D.S., M.B.A., M.S., an associate professor of dentistry at the University of the Pacific, said, "I know what Rella is doing pretty well, and I don't disagree with her. In an ideal world we would like to work in a sterile environment, so disinfection of the tooth preparation is a step forward. Since the studies have not been done, we are not yet where we can say we have to do this."
Dr. Young uses a chlorhexidine cavity cleaner by Ultradent or sodium hypochlorite to disinfect his preparations. He hesitates to use glutaraldehyde because its interaction with glass ionomers has not been studied.
Christensen acknowledged that the interaction of glutaraldehyde and glass ionomers is unknown, but said the disinfectant "probably doesn't affect resin-modified glass ionomers adversely." She said interactions between glass ionomers and sodium hypochlorite and chlorhexidine have not been thoroughly researched either. She noted that chlorhexidine is not cleared by the FDA as a disinfectant for tooth preparations. Sodium hypochlorite did not have to go though the clearance process because it was widely available before the FDA was founded.
Another important question is whether placing restorations cuts off the nutrient flow to bacteria. "Studies have shown that if you seal in bacteria and leave in some decay, the carious lesion does not progress," said Dr. Young. "If they can't ferment carbohydrate, they can't create acids, and if they can't create acids, they can't demineralize the tooth."
Christensen said her research called into question the effectiveness of entombing the organisms. "With time, everything leaks," she said. "And what if the nutrient source was the dentin?"
Caries do develop under some sealants and restorations, she said. "I think it's a mistake to have organisms present that cause the caries. I am not aware of research showing that these organisms cannot continue to sustain themselves and cause recurrence of the disease later."
In her article, she identified Gluma by Heraeus Kulzer, Glu/Sense by Centrix, G5 by Clinician's Choice, and MicroPrime G by Danville Materials as some commercially available brands of 5% glutaraldehyde, 35% HEMA.
As for a protocol, Christensen recommends the following:
- Prepare the tooth as usual.
- Just before the cement, resin-modified glass ionomer, sealant, or bonding agent, apply the glutaraldehyde with a microbrush (avoid soft tissue).
- Wait 60 seconds.
- Suction out the glutaraldehyde (Christensen advises against rinsing with water).
- Repeat steps 2 through 4 (to make sure all areas of the preparation have been contacted).
- Proceed as usual.
Sound like a hassle? "If it's good for the patient, the trouble and expense don't matter," said Christensen.