After having jaw surgery, a 30-year-old woman developed a very rare neural eating disorder that led her to lose consciousness and experience amnesia while consuming food, according to a case report published in Advances in Oral and Maxillofacial Surgery.
The case suggests that late presentation of swallowing syncope, which is associated with severe transient heart disorders, may be a postsurgical complication of jaw surgery, the authors wrote.
"It is possible that orthognathic surgery induced swallow syncope of neurogenic origin," wrote the authors, led by Belmiro Cavalcanti do Egito Vasconcelos, PhD, of the University of Pernambuco in Brazil (Adv Oral Maxillofac Surg, August 11, 2022).
30-year-old woman with throat spasms
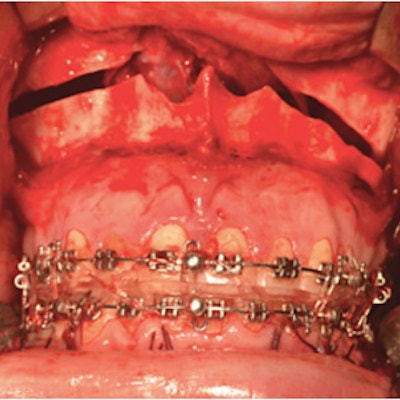
The healthy patient, who had a skeletal class III deformity, underwent jaw surgery with a LeFort I osteotomy with horizontal maxillary advancement, mandible retraction, and clockwise rotation through sagittal osteotomies. In addition, she underwent a surgical procedure to reshape her chin, according to the report.
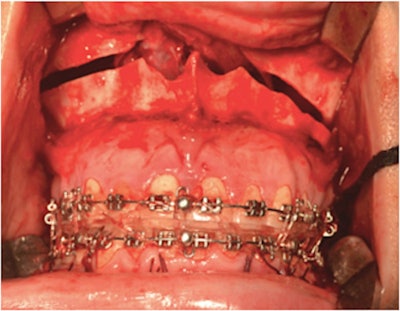 The woman underwent a LeFort I osteotomy with horizontal maxillary advancement. Images courtesy of Vasconcelos et al. Licensed by CC BY 4.0.
The woman underwent a LeFort I osteotomy with horizontal maxillary advancement. Images courtesy of Vasconcelos et al. Licensed by CC BY 4.0.About seven months after the procedures, she had occlusal stability and no abnormal bone displacement, but she was experiencing malaise and throat spasms during meals. Additionally, the woman started having moderate pain in her oropharynx and hypopharynx during chewing and swallowing, as well as dizziness with a loss of balance and visual impairment, the authors wrote.
Over the next three months, her condition evolved. During one meal, she experienced up to five events of syncope, with a loss of consciousness and amnesia. Clinical and hematological exams showed nothing new, but a heart evaluation showed she had a rare cardiac alteration, suggestive of swallow syncope with asystole, they wrote.
A Holter monitor test revealed the woman had an average heart rate of 80 beats per minute, with a minimum of 57 beats per minute. Her symptoms were linked to the presence of a 5.4-second pause due to a high-grade block, the authors wrote.
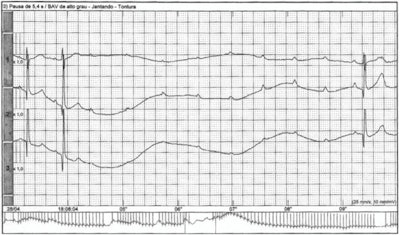 An electrocardiogram revealed that the woman's symptoms were related to the presence of a 5.4-second pause due to a high-grade block.
An electrocardiogram revealed that the woman's symptoms were related to the presence of a 5.4-second pause due to a high-grade block.Though she improved significantly once she began taking bendroflumethiazide, her symptoms weren't gone. After taking the medication for six months, a permanent pacemaker was implanted, which resolved all episodes of unconsciousness and dizziness, they wrote.
Extremely unusual and deadly
Swallow syncope is mediated by a vagal reflex and is characterized by a loss of consciousness while eating solid food. It is associated with life-threatening bradyarrhythmia and low blood pressure. Usually, it occurs after periods of fasting.
Diagnosis and management of swallow syncope often are delayed because it can be difficult to diagnose. When swallow syncope is suspected, the authors recommend using a multidisciplinary approach to treatment planning.
Past studies have shown that orthognathic surgery can possibly result in a neurofunctional lesion and impairment of the vagus nerve. Additionally, the Le Fort I maxillary osteotomy has been linked to palsies of the vagus and accessory nerves, causing difficulty with swallowing, cough, and vocal cord paralysis, the report's authors wrote.
Despite the structural changes that occur because of orthognathic surgery, the procedure does not completely change the myofunctional pattern or significantly alter those structures related to swallowing.
"In this context, the late manifestation of clinical symptoms suggests that the surgical technique was not the primary etiology of this pathology, but rather predisposed the patient to this disorder," Vasconcelos and colleagues wrote.



















