The goals of dental implant therapy have evolved beyond attaining osseointegration of the implant to also enhancing and maintaining the soft-tissue aesthetics around the implant. This helps maintain the long-term effectiveness of the surgery and the aesthetics of the oral cavity and jawline. However, if a patient needing an oral implant has an infection, current practice has been to wait until the infection is healed. However, as this delay in treatment lowers the success rates from about 100% to about 92%, finding a way to place an implant in those patients who do have an infection may boost success rates.
According to a case study in the Journal of Oral Implantology (April 2014, Vol. 40: 2, pp. 211-216), an international team of clinicians, led by Aladdin Al-Ardah, DDS, from Loma Linda University School of Dentistry, has devised a new procedure that may allow immediate placement of implants in patients with an oral infection. This technique uses a single incision for access combined with localized antibiotics to treat the infection. The goal is to allow immediate implantation with a bone graft harvested from a portion of the patient's own lower jaw.
In this case, a 43-year-old woman presenting with a front-tooth infection of seven-months duration underwent a root canal and antibiotics. However, as her symptoms persisted, it was recommended that the tooth be removed.
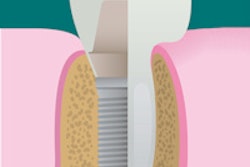
The patient had a thin gingival biotype with mesial and distal papilla grade 2 scores, according to interdental papilla loss classification, the authors reported. The patient's bone sounding was 4 mm on the distal side of tooth No. 9, 6 mm on the mesial side of tooth No. 10, 10 mm on the midbuccal side, 8 mm on the distal side of tooth No. 10, and 5 mm on the mesial side of tooth No. 11. The authors noted her tooth shape as triangular and she had a high smile line with a symmetrical gingival zenith.
Practitioners used a single vertical incision to harvest the bone from the symphysis area running parallel to the muscle fibers. The advantages of this technique are that it eliminates the detachment of muscles and reduces the risks of neurosensory disturbance, chin ptosis, and patient discomfort. However, the apex of the anterior teeth must be mapped carefully, and compared with the classical approach, the amount of harvested bone is limited to one or two trephines because of the limited access mandated by the single vertical incision, the authors noted. The patient's infection was treated with localized antibiotics.
Grafting procedures
For grafting procedures, autogenous bone graft has been a gold standard because of its osteogenic, osteoinductive, and osteoconductive capacities. The mandibular symphysis is often used as a donor site because up to 10 mL of corticocancellous bone graft can be harvested, which eliminates the need for extraoral sources. While this has many advantages, there can be complications, including postoperative morbidity and patient discomfort. Chin ptosis also is a concern because of the disturbance of the muscle attachments resulting from harvesting bone from this area, the authors reported.
The practitioners' dilemma was whether to place the implant after performing the extraction, followed by the bone graft. This strategy could lead to hard- and soft-tissue changes. While immediate implant placement and provisionalization might have preserved the soft-tissue contour, this patient's buccal abscess had not been responsive to systemic antibiotics, which could complicate the stability of implant placement and jeopardize the bone graft needed to repair the buccal defect.
Six months after placement, a bone sounding was done. The rates of healing included 3 mm on the distal side of tooth No. 9, 3.5 mm on the mesial, 3 mm on the midbuccal, 3.5 mm on the distal side of implant No. 10, and 3.5 mm on the mesial side of tooth No. 11.
A final impression also was made at this time. A custom zirconia abutment (Procera, Nobel Biocare) was fabricated and a cement-retained ceramic crown was processed and cemented. The importance of a high standard of oral hygiene and tooth brushing and dental flossing techniques were reinforced. Chlorhexidine (Periodex, 0.12%, 3M ESPE) mouth rinse was prescribed once daily for seven consecutive days.
During three-year follow-up (until the patient moved), no significant soft- or hard-tissue changes were observed, the authors noted.