SARS-CoV-2 may cause epithelial changes to the upper surface of the tongue, causing patients with COVID-19 to experience bad breath, according to a letter to the editor published on November 29 in Special Care in Dentistry.
The alterations on the tongue surface may occur via binding with angiotensin-converting enzyme 2 (ACE2) receptors, which are present throughout the oral mucosa with the greatest expression on the tongue. These tongue alterations, in turn, can lead to halitosis. Other infections caused by the novel coronavirus may also play a role, the authors wrote.
"Bacterial co-infections arising from SARS-CoV-2 may have a role in modulating the oral environment to [favor] the proliferation of species comprising the halitosis-associated microbiota and broader periodontopathic gram-negative bacteria," wrote the group, led by Dr. Abanoub Riad of the Czech National Centre for Evidence-Based Healthcare and Knowledge Translation.
Another link in the chain
Respiratory, otolaryngologic, and gastrointestinal conditions can alter salivary characteristics and the upper surface of a person's tongue, resulting in bad breath. Evidence suggests the mouth is a powerful source of SARS-CoV-2 infection and transmission, and the novel coronavirus may also be linked to tongue ulcers, angular cheilitis, and other oral manifestations. Therefore, it is not surprising that there may be a link between COVID-19 and halitosis.
Riad and colleagues reviewed clinical and lab data from 18 patients who were diagnosed with COVID-19 and began experiencing halitosis during their infections. They had no other relevant medical history. Two of the patients had poor oral hygiene, and another had an intraoral ulcer. Approximately 78% of the patients were women, and many had differing symptoms, including fever and loss of smell or taste.
The researchers used a detector to estimate the number of volatile sulfur compounds (VSCs) in parts per billion (ppb) in the patients' breath. Initially, the mean halitosis intensity was 203.89 ± 95.56 (range, 100-420) ppb, which confirmed that all patients had physiological halitosis. Twelve patients used a mouthwash that contained lidocaine, chlorhexidine, and prednisolone, among other ingredients, and six patients used a chlorhexidine gluconate 0.3% mouthwash. After a month, the mean halitosis intensity score was 68.75 ± 30.96 (range, 20-120) ppb. Two patients didn't return for follow-up.
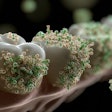
Tongue changes
The surface of the tongue may have been altered and caused halitosis due to medications that patients received to treat or prevent secondary infections. Some of the patients were taking acetaminophen, ibuprofen, prednisolone, or chloroquine. Bad breath is a side effect of acetaminophen, ibuprofen, and chloroquine, the authors noted.
Wearing a mask to prevent the spread of the novel coronavirus also may cause mouth breathing, which can lead to dry mouth and bad breath. In addition, wearing a mask may have helped people realize that they had bad breath, according to the authors.
Riad and colleagues believe these cases prove that this area should be studied further.
The cases warrant "larger epidemiological studies to accurately estimate the prevalence of halitosis among COVID-19 patients and to further investigate its possible etiologies that may be linked either directly, or indirectly, to SARS-CoV-2," the authors wrote.