Titanium exposure and scaling have become suspects in the worsening of peri-implantitis, but the actual concentration of titanium in tissues surrounding an implant with this condition has remained unclear. To learn more, researchers examined the titanium contained in tissue from patients with severe peri-implantitis.
The investigators analyzed biopsy contents from patients with peri-implantitis and control subjects with periodontitis. They found that both types of tissue contained metal fragments but only the peri-implantitis tissue included titanium. Their study was published in the Journal of Oral Rehabilitation on October 16.
"The high titanium content in peri-implant mucosa has the potential to aggravate inflammation, which might reduce the prognosis of treatment interventions," wrote the authors, led by Mattias Pettersson, PhD, the senior dental officer in the prosthetic dentistry division of the Umeå University Department of Odontology in Sweden.
Titanium and peri-implantitis?
Some researchers believe peri-implantitis is an infectious disease caused by the presence of bacterial biofilm on an implant, while others suggest it is due to an aggravated foreign body response to the implant, the authors noted.
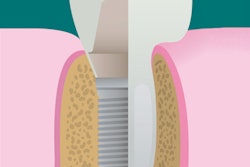
Mechanical biofilm removal from the implant surface is among the treatments used for peri-implantitis, but this may cause the release of titanium particles in tissue and aggravate peri-implantitis, according to previous research. Additionally, current titanium implants have rougher surfaces thought to enhance tissue integration and osseointegration, and surface enlargement of titanium implants has been found to increase the release of metal debris during implantation.
“The high titanium content in peri-implant mucosa has the potential to aggravate inflammation, which might reduce the prognosis of treatment interventions.”
An inflammatory process caused by microorganisms around an implant combined with titanium particles in the peri-implant mucosa could be devastating, the study authors noted. Since the concentrations and structures of titanium in tissues surrounding an implant with severe peri-implantitis are unknown, the researchers of the current study examined the titanium content of biopsies from patients with severe peri-implantitis and the gingiva of controls with periodontitis and without titanium exposure.
They recruited consecutive patients referred for surgical treatment of severe peri-implantitis or periodontitis in Sweden. The researchers defined severe peri-implantitis as bleeding on probing with loss of supporting bone exceeding four threads or a probing depth of 7 mm or greater, and they defined severe periodontitis as bleeding on probing and a probing depth greater than 7 mm.
They collected data on seven topics from 13 study participants with peri-implantitis and 11 with periodontitis:
- Tobacco use
- Periodontal history
- Medication use
- Type of prosthetic replacement (full arch, partial arch, or single tooth)
- Total number of implants and number lost
- Titanium in the prosthetic material (commercial pure or alloy)
- Infection signs, such as bleeding on probing with or without purulent exudate
Both patient groups underwent surgery with removal of granulation tissue, calculus, and biofilm, and implant surfaces underwent cleaning with an ultrasonic scaler, gauze dressing, and saline. During surgical treatment, investigators obtained tissue from a peri-implant or periodontal pocket for analysis with inductively coupled plasma mass spectrometry.
The researchers also analyzed biopsies from two additional patients with severe peri-implantitis and two with severe periodontitis. They studied granulation tissue removed from the peri-implants and periodontal soft tissue during surgery using light microscopy, scanning electron microscopy, and transmission electron microscopy.
They found that more than 92% of the prosthetic reconstructions were titanium. All participants with peri-implantitis lost at least one implant, despite having treatment for the condition. Biopsies from peri-implantitis tissue had very high mean titanium concentrations of 98.7 µg/g compared with periodontitis control tissue with concentrations of 1.2 µg/g (p < 0.001). Low concentrations in periodontitis tissue may be due to exposure in toothpaste or food, as well as through environmental exposure, such as in cosmetics, the authors explained.
The researchers identified particulate metal in both peri-implantitis and periodontitis biopsies, but element analyses confirmed the presence of titanium only in peri-implantitis tissue.
"Our data in the present study support the finding that titanium is the main foreign body material identified in peri-implantitis biopsies," the authors wrote.
The origin of the titanium found in peri-implant mucosa is unknown but could derive from scaling of the implant and corrosion, they explained. They questioned whether scaling should be performed on implants and suggested that other techniques for decontamination of their surfaces are needed.
Enhanced immunological response
The study was limited because no comparison was performed between the titanium contents of peri-implant mucosa and the tissue of healthy implants since it would be unethical to perform biopsies on patients with healthy implants, the authors noted.
Better understanding of the origins of titanium in peri-implant tissue and how to reduce it may be key to understanding and treating peri-implantitis, they wrote.
"We support the hypothesis that peri-implantitis is an infectious disease induced by a bacterial biofilm on the implant surface, but the presence of titanium particles in the peri-implant tissue might further enhance the immunological response and aggravate the loss of supporting bone," the authors concluded.