Biofeedback (BF) may be an effective educational tool for managing temporomandibular disorders (TMDs) and improving patients’ well-being, according to a recently published review in BMC Oral Health.
Though biofeedback did not reduce pain as well as other treatments, it was equally effective, and it may provide added value by addressing psychological aspects associated with TMD, the authors wrote.
“This systematic review and network meta-analysis highlight the exploratory potential of BF as a possible educational intervention for patients with TMD, offering benefits beyond pain relief by addressing the psychological and biobehavioral aspects of the disorder,” wrote the authors, led by Ada María González-González of the Adavall Physiotherapy and Rehabilitation Clinic in Valladolid, Spain (BMC Oral Health, September 2, 2025, Vol. 25, 1395).
Researchers conducted a systematic review and meta-analysis to assess the effectiveness of BF as an educational treatment for TMD. The review focused on clinical trials that used BF as a therapeutic intervention in patients with TMDs. Educational BF was defined as an approach designed to improve self-regulation, behavioral change, or physiological awareness through real-time feedback and therapist guidance, the authors wrote.
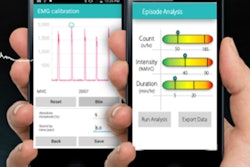
Interventions included strategies where patients learned to adjust muscle activity using visual, auditory, or vibratory cues, that was sometimes combined with cognitive or behavioral techniques. Studies were excluded if BF was used passively, only during sleep, or without patient interaction and feedback interpretation.
The review analyzed nine studies with varied patient groups, treatment protocols, and methods, most of which showed a low risk of bias. The meta-analysis found no significant differences, but biofeedback showed moderate clinical effects compared with no intervention, suggesting potential benefits such as increased body awareness and reduced parafunctional habits, or involuntary behaviors, they wrote.
However, biofeedback ranked lower than occlusal splints in effectiveness, indicating it may be best as a complementary rather than primary treatment.
Studies highlighted psychological benefits, with biofeedback linked to improvements in depression, anxiety, and coping skills, particularly when combined with cognitive-behavioral therapy (CBT). Overall, the findings support biofeedback in addressing both the physical and psychological aspects of TMD.
The study had limitations, including that some studies combined BF with CBT or occlusal splints, making it difficult to determine whether improvements were due to BF alone or the added interventions, the authors added.
“Although methodological limitations exist, these findings support the further exploration of BF in clinical practice and research settings,” they concluded.