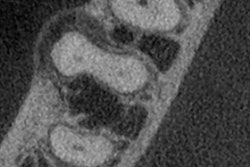
 Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
DrBicuspid publishes a new case study weekly. To test your dental expertise, first, please log in. If you don't have a login, create one. Each case comprises a history, quiz, and discussion section. An answer key is provided at the end of the case study.
A 63-year-old man presented to the oral surgeon after being referred by his family dentist because of an unusual radiolucency at the inferior border of the right mandible. Patient was asymptomatic. His past medical history included hypertension and high cholesterol, and he was taking lisinopril.
Log in to view the full article
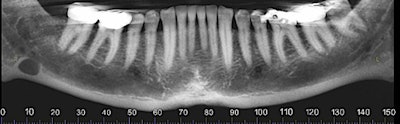 Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
DrBicuspid publishes a new case study weekly. To test your dental expertise, first, please log in. If you don't have a login, create one. Each case comprises a history, quiz, and discussion section. An answer key is provided at the end of the case study.
History
A 63-year-old man presented to the oral surgeon after being referred by his family dentist because of an unusual radiolucency at the inferior border of the right mandible. Patient was asymptomatic. His past medical history included hypertension and high cholesterol, and he was taking lisinopril.
The extra- and intraoral exams were within normal limits.
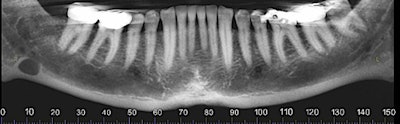
The oral surgeon ordered a cone-beam CT (CBCT) exam. Click images below to enlarge. In order: reformatted panoramic radiograph and cropped image of the area of interest, coronal view of the posterior right mandible (the inferior alveolar canal in red), and 3D reconstructed image of the posterior right mandible.
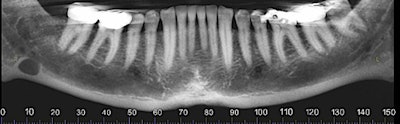 Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
Figure 1: Reformatted and cropped panoramic film. All images courtesy of Dr. Juan F. Yepes.
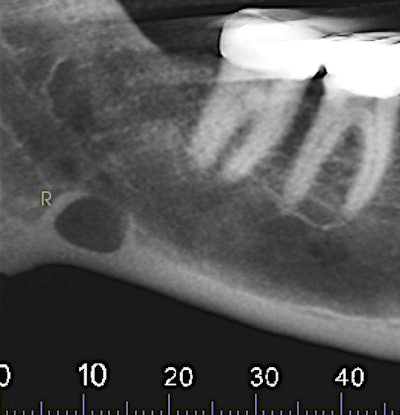 Figure 2: Reformatted and cropped panoramic film.
Figure 2: Reformatted and cropped panoramic film.
 Figure 3: Coronal view of the posterior right mandible (the inferior alveolar canal is highlighted by red dot).
Figure 3: Coronal view of the posterior right mandible (the inferior alveolar canal is highlighted by red dot).
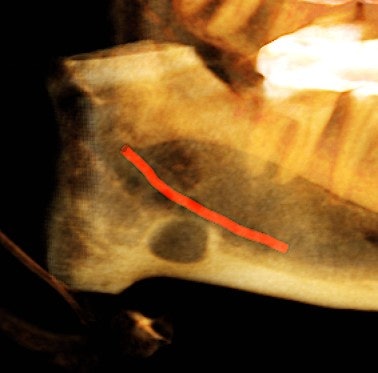 Figure 4: Coronal view of the posterior right mandible (the inferior alveolar canal highlighted in red) and 3D-reconstructed image of the posterior right mandible.
Figure 4: Coronal view of the posterior right mandible (the inferior alveolar canal highlighted in red) and 3D-reconstructed image of the posterior right mandible.
1. Which of the following is the LEAST LIKELY preliminary diagnosis?
A. Radicular cyst
B. Idiopathic bone cavity
C. Hypertrophic lymph node
D. Tumor metastasis
2. The oral surgeon consulted with an oral radiologist, who provided an interpretation report. The following is from the report:
There is a hypodense lesion (radiolucent) that is well-defined, well-corticated, oval in shape, 8 x 6 mm, located at the posterior right mandible, and distal to tooth #32. The lesion is located below the inferior alveolar canal. No expansion is observed in the cross-sectional views. No calcifications are observed inside the lesion.
Based on the images and the radiology report, which of the following is the most likely diagnosis?
A. Ameloblastoma
B. Cementoblastoma
C. Idiopathic bone cavity
D. Metastasis
E. Stafne bone defect
3. Which of the following is the most likely next step?
A. Incisional biopsy
B. Excisional biopsy
C. Prescription of antibiotics
D. Surgical excision of the lesion
E. None of the above
Diagnosis: Stafne bone defect
4. The oral surgeon explained to the patient the diagnosis and recommended periodic follow-up.
Which of the following statements is true about Stafne bone defect?
A. They typically occur in patients between the ages of 20 and 30 years old.
B. Advance imaging (such as MRI or CT) is usually recommended.
C. They most commonly occur in the posterior maxilla.
D. None of the above is true.
Discussion
The Stafne bone defect (SBD), or salivary gland defect, was first described by Edward Stafne, DDS, in 1942. The exact etiology is not clear. It is suggested that the cavity is the result from a defect of normal bone deposition in the region previously occupied by cartilage. However, probably the most accepted hypothesis is that the cavity develops as a result of localized pressure atrophy of the lingual surface from the adjacent salivary gland.
The majority of cases are located in the posterior mandible, between the mandibular angle and first mandibular molars and below the inferior alveolar canal. They are asymptomatic, with a slightly predilection for men between 50 and 70 years old. The diagnosis is incidental, since patients do not usually present with clinical symptoms.
From the radiographic perspective, Stafne bone defects are radiolucent lesions, well-defined and well-corticated, oval in shape, and located below the inferior alveolar canal. No expansion is usually observed in the coronal views.
The differential diagnosis includes benign and malignant lesions; however, the location below the inferior alveolar canal is an anatomical landmark that helps to differentiate a Stafne bone defect from odontogenic lesions (usually located above the inferior alveolar canal).
No treatment is usually necessary; however, atypical lesions may require advanced imaging and biopsy.
Reference
- Greenberg M, Glick M, Ship J. Burket’s Oral Medicine. 11th ed. Hamilton, Ontario; 2008: BC Decker Inc.
- Neville B, Damm D, Allen C, Bouquot J: Oral and Maxillofacial Pathology. 3rd ed. St Louis, Missouri: Mosby-Elsevier: 2009.
Answer key
- A; radicular cyst.
- E; Stafne bone defect.
- E; none of the above.
- D; none of the above is true.