
Significantly more Californians visited the emergency room (ER) for dental-related problems after the state cut dental benefits for adults enrolled in Medicaid, according to a new journal article. The authors hope policymakers will consider adding comprehensive dental coverage to other state's plans because of the results.
The study, which was published in the May 2015 edition of Health Affairs, looked at dental-related emergency department (ED) visits by adults enrolled in Medicaid before and after California cut comprehensive dental benefits in July 2009. Lead author Astha Singhal, a doctoral candidate in the department of preventive and community dentistry at the University of Iowa College of Dentistry, and colleagues found the cuts correlated with a 32% increase in ED visits, costing the state Medicaid program an additional $1.25 million per year.
"Our results provide evidence that the elimination of dental benefits for Medicaid adult enrollees led to an immediate and significant increase in dental ED visits by Medicaid-enrolled adults in California," the authors wrote (Health Affairs, May 2015, Vol. 34:5, pp. 749-756).
Dental coverage cuts directly affect ED visits
When left untreated, dental diseases impact peoples' productivity and quality of life. Those without dental coverage may be forced to visit an emergency department for dental problems, but EDs, while an important part of the healthcare safety net, are not trained to handle dental diseases.
“Our results provide evidence that the elimination of dental benefits for Medicaid adult enrollees led to an immediate and significant increase in dental ED visits.”
"As a result, the vast majority of patients who visit an ED with a dental problem do not receive definitive dental treatment," Singhal and colleagues. "Instead, they receive only prescriptions for painkillers, antibiotics, or both."
In addition, when those enrolled in Medicaid visit EDs for dental-related emergencies, it adds to the state's Medicaid costs. The researchers set to find out whether California's intent of limiting Medicaid costs was at least partially offset by an increase in ED visits.
They looked at adults ages 21 and older who were enrolled in Medicaid at any time from 2006 to 2011. They gathered data from the State Emergency Department Databases, which collects information for all ED visits that do not result in hospital admission, and the California Department of Health Care Services. Singhal and colleagues used an interrupted time-series study design with control outcome variables to minimize the possibility of outside events, like the 2008 recession, that could affect the study's results.
The authors found that there were about 10 more dental ED visits per 100,000 Medicaid enrollees per month and that annual costs for dental ED visits increased by 68% after California cut comprehensive dental coverage. The change significantly impacted young people, those living in metropolitan areas, and multiple race and ethnic groups.
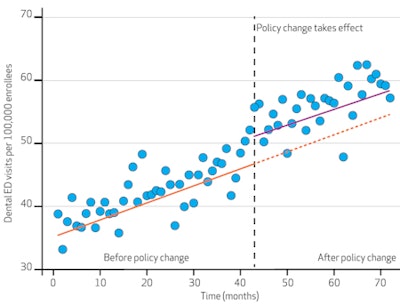 Dental ED visits significantly increased after California cut dental insurance for adults enrolled in Medicaid in 2009. Source: Authors' analysis of data for the period 2006-2011 from the California State Emergency Department Database. Notes: California eliminated Medicaid adult dental coverage in July 2009 (the 43rd month of the study period, indicated by the dashed vertical line). The solid orange and purple lines represent the best fit regression line for actual ED visits. The orange dashed line represents the expected rate of ED visits in the absence of the policy change. The change in intercept was significant. Image courtesy of Health Affairs.
Dental ED visits significantly increased after California cut dental insurance for adults enrolled in Medicaid in 2009. Source: Authors' analysis of data for the period 2006-2011 from the California State Emergency Department Database. Notes: California eliminated Medicaid adult dental coverage in July 2009 (the 43rd month of the study period, indicated by the dashed vertical line). The solid orange and purple lines represent the best fit regression line for actual ED visits. The orange dashed line represents the expected rate of ED visits in the absence of the policy change. The change in intercept was significant. Image courtesy of Health Affairs.Cutting dental benefits saves and costs states
After California cut comprehensive adult Medicaid dental care, the state spent an average of $1.25 million per year for dental-related ED visit costs. However, the state saved a total of $246 million in the first year alone after the cuts. While the difference is off-putting, the authors urge states to consider other, hidden costs associated with not providing dental coverage.
"Policymakers should think of these costs in terms of cost-effectiveness rather than of cost savings per se," they wrote. "To get the total costs, we would need to capture the costs associated with increases in hospital admissions and in care sought at other nontraditional venues for dental care ... and the costs associated with loss of productivity and worsening quality of life due to untreated dental disease."
Emergency room visits for dental problems were also significantly increasing even before California cut Medicaid coverage, a trend that is happening elsewhere in the U.S., according to the authors. They suggest this trend could be due to low Medicaid participation by private dentists, increasing income inequality, slow economic growth, and low reimbursement rates.
"Even before the policy change, nonelderly Medicaid adults had a much greater rate of dental ED visits than nonelderly uninsured," the authors wrote. "Moreover, the California Medicaid program's reimbursement rates are among the lowest nationally," which has led to a decline in dentist participation from 40% in 2003 to 24% in 2010, they added.
It should also be noted that California reinstated partial adult dental benefits in 2014, once the economy began to recover, and the authors believe other states should follow suit.
"The results from California provide relevant and valuable evidence to support dental coverage for Medicaid adult enrollees in other states that are considering a policy change," Singhal and colleagues concluded. "Our results provide evidence that eliminating Medicaid adult dental coverage leads to a significant increase in dental ED visits and associated costs."



















