Imaging helped treat a 61-year-old man with the rare coexistence of calcium pyrophosphate crystal deposition and a synovial tumor in the temporomandibular joint (TMJ). The case report was published in BMC Oral Health.
Thanks to technological advancements in radiology, synovial chondromatosis, a noncancerous type of tumor that arises in the lining of a joint known as the synovium, in the TMJ isn't as rare as once thought, but it is far from common. However, calcium pyrophosphate crystal deposition of the TMJ is considered rare, with only a few cases reported in the literature, the authors wrote.
 The red arrow on the patient's dental x-ray indicates a large mass with a gravel-like appearance and calcified foci around the lower jaw condyle with medial extension into the infratemporal fossa of the right TMJ. Images courtesy of Ntege et al. Licensed by CC BY 4.0.
The red arrow on the patient's dental x-ray indicates a large mass with a gravel-like appearance and calcified foci around the lower jaw condyle with medial extension into the infratemporal fossa of the right TMJ. Images courtesy of Ntege et al. Licensed by CC BY 4.0.The man underwent surgery and made a complete recovery. Had he not been treated, he could have experienced continued acute pain and accelerated joint damage.
"However, the coexistence of both CPPD (calcium pyrophosphate crystal deposition) and SC (synovial chondromatosis) in the temporomandibular joint remains a rare condition," wrote the case report's authors, led by Dr. Edward Hosea Ntege of the University of the Ryukyus in Japan. (BMC Oral Health, December 31, 2022, Vol. 22, 662).
A 61-year-old man with TMJ pain and trismus
After experiencing pain in the right cheek and restricted mouth opening for more than six months, a 61-year-old man was referred to an oral and maxillofacial surgery department. He was referred by his primary doctor after the frequency and intensity of pain increased and he no longer responded to nonsteroidal anti-inflammatory drugs. The man had controlled type 2 diabetes, high blood pressure, and a history of bruxism, according to the report.
An exam revealed the man had mild swelling at the right preauricular region and a limited mouth opening of 15 mm that was accompanied by myofascial pain in the right TMJ region. Also, the man had an excessive malocclusion and incisal tooth wear of the upper and lower jaws. However, there were no signs of a mass or infection, the authors wrote.
Dental x-rays showed horizontal bone resorption in the upper and lower jaws and extensive calcificationlike opacities in the right TMJ while magnetic resonance imaging (MRI) showed the dilation of the upper and lower joint spaces with differing levels of hypointensity. However, there was no observable disc dislocation in the joint on the right side, and the left side showed nothing abnormal, they wrote.
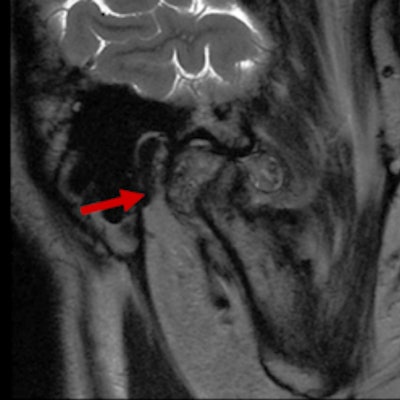
 The patient's preoperative MRI images. (A) Sagittal T1-weighted sequence of the right TMJ shows a fluid-filled mass expanding within the joint space, as well as multiple loose bodies. (B) A coronal proton density-weighted sequence shows a heterogeneous signal intensity tissue mass within the capsule of the right TMJ between the right glenoid fossa and the mandibular condyle (red arrow).
The patient's preoperative MRI images. (A) Sagittal T1-weighted sequence of the right TMJ shows a fluid-filled mass expanding within the joint space, as well as multiple loose bodies. (B) A coronal proton density-weighted sequence shows a heterogeneous signal intensity tissue mass within the capsule of the right TMJ between the right glenoid fossa and the mandibular condyle (red arrow).The man underwent a computed tomography scan that revealed an area of hard tissue that measured 38 mm, multiple rice-grain opacities around the right mandibular condyle, and osteosclerosis of the right articular head with no observable bone resorption, the authors wrote.
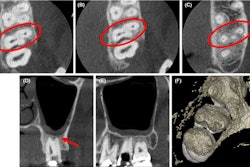
 The patient's preoperative CT images. (A) The axial view shows large intra-articular localized calcified lesions that abut the articular surface of the mandibular condyle of the right TMJ. (B) The coronal view of the right TMJ indicates partial attachment of the calcified mass to the superior aspect of the mandibular condyle and cranial base.
The patient's preoperative CT images. (A) The axial view shows large intra-articular localized calcified lesions that abut the articular surface of the mandibular condyle of the right TMJ. (B) The coronal view of the right TMJ indicates partial attachment of the calcified mass to the superior aspect of the mandibular condyle and cranial base.Based on the imaging and clinical features, the differential diagnosis was a tumor or a tumorlike disease. To get a definitive diagnosis, a biopsy was done. Upon opening the superior articular space, a mass covered with a fibrous capsule was seen. The mass, which was surrounding the mandibular condyle and had numerous white, cartilagelike hard tissues and chalklike soft tissues of mixed sizes, was removed and sent to the lab for analysis. Results showed that the mass was formed by aggregates of basophilic crystal deposits surrounded by a giant cell reaction, the report's authors wrote.
 (A) An image of cartilagelike structures of mixed sizes within a hyperplastic fibrous tissue that was removed from the patient. (B) A bone and chalklike tissue specimen that was removed from the patient.
(A) An image of cartilagelike structures of mixed sizes within a hyperplastic fibrous tissue that was removed from the patient. (B) A bone and chalklike tissue specimen that was removed from the patient.Since the patient had no history of trauma and imaging revealed joint effusion with multiple calcified loose bodies in a tumorlike lesion with a well-defined border surrounding the lower jaw condyle of the right TMJ and the loose bodies were confirmed by histopathology, the patient was diagnosed with calcium pyrophosphate crystal deposition and synovial chondromatosis, according to the case report.
The man underwent surgery to have the lesions, as well as the synovial tissue surrounding the TMJ, removed to prevent recurrence and improve his jaw function. Two years after the procedure, he had no recurrence, they wrote.
Understanding these conditions
Calcium pyrophosphate crystal deposition is described as the buildup of these crystals in various intra-articular and/or periarticular tissues, resulting in acute noninfectious inflammatory and degenerative chronic joint diseases and calcifications in cartilage. Most often, crystal deposition occurs in large joints such as the hip.
Synovial chondromatosis is a rare tumor that is linked to metaplastic proliferation of cartilaginous nodules within the synovium. Commonly, it manifests as intra-articular loose bodies. In approximately 1 per 100,000 people, loose bodies form within extra-articular spaces. Both conditions have the potential to cause acute pain and joint damage.
Despite the advances in imaging, as well as interest in research and application of several different diagnostic approaches, clinicians have difficulties diagnosing TMJ diseases, they wrote.
"We report the case of a 61-year-old man to expand the body of literature on these unusual coexisting arthropathies of the TMJ," Ntege and colleagues wrote.