Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
DrBicuspid publishes a new case study weekly. To test your dental knowledge, first, please log in. If you don't have a login, create one. Each case comprises a history, quiz, and discussion section. An answer key is provided at the end of the case study.
Log in to view the full article
 Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
DrBicuspid publishes a new case study weekly. To test your dental knowledge, first, please log in. If you don't have a login, create one. Each case comprises a history, quiz, and discussion section. An answer key is provided at the end of the case study.
History
A 25-year-old man was referred to the oral surgeon by his dentist because of a "lesion" on the left side of his posterior mandible. The patient was asymptomatic. There were no signs of parestheia or swelling.
The patient's past medical history was significant for anxiety and chronic sinus infections. The intraoral and extraoral exams were normal.
The oral surgeon ordered a cone-beam computed tomography (CBCT) scan. Below are the following images:
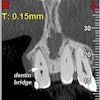
- A cropped, reformatted pano film of the left mandible
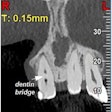
- CBCT coronal images of the left posterior mandible
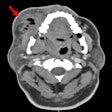
- A CBCT coronal view of the posterior mandible
 Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
Figure 1: Cropped, reformatted panoramic film of the left mandible.Images courtesy of Dr. Juan F. Yepes.
 Figure 2: CBCT coronal images of the left posterior mandible.
Figure 2: CBCT coronal images of the left posterior mandible.
 Figure 3: CBCT, coronal view of the posterior mandible.
Figure 3: CBCT, coronal view of the posterior mandible.
1. The oral surgeon wrote a preliminary diagnosis based on the images and the clinical presentation. What is the most likely preliminary diagnosis?
- Idiopathic bone cavity
- Ameloblastic fibroma
- Ameloblastic fibro-odontoma
- Odontogenic keratocyst
The oral surgeon consulted with an oral and maxillofacial radiologist who evaluated the images and provided an interpretation report. The following paragraph is from the report:
There is a large hypodense lesion (radiolucent), well defined and corticated, extending from the mesial aspect of tooth #17 to the periapical area of tooth #22. The lesion goes from the inferior cortex of the mandible to the alveolar ridge of teeth #18 and #19, the middle third of the root of tooth #20, and the apical third of the root of tooth #21. There is evidence of significant expansion in the coronal and axial projections. No calcifications are observed within the lesion. No periosteal reaction is observed (lingual or buccal). There is no radiographic evidence of perforation of the buccal or lingual walls of the lesion.
There is no radiographic evidence of root resorption or teeth displacement associated with the lesion. No gross caries is present in the teeth involved in the lesion. The inferior alveolar canal is well visualized and displaced buccally-apically by the lesion.
2. Based on the interpretation report, what is the most likely diagnosis?
- Adenomatoid odontogenic tumor
- Cemento-osseous dysplasia
- Dentigerous cyst
- Unicystic ameloblastoma
- Idiopathic bone cavity
A few weeks later, the oral surgeon performed an incisional biopsy. The histopathology report was available a few days later. The following remarks are from the histology report:
The microscopic examination reveals a cystic lesion mainly lined by a thin layer of nonkeratinizing stratified squamous epithelium. There is minimal inflammation in the thick fibrous connective tissue wall. Invading epithelium demonstrates a basal layer of columnar cells with hyperchromatic nuclei that shows reverse polarity and basilar cytoplasmic vacuolization. Suprabasal epithelial cells are loosely cohesive, resembling stellate reticulum.
3. Based on the clinical presentation, images, and histopathology report, what is the most likely diagnosis?
- Unicystic ameloblastoma
- Idiopathic bone cavity
- Myxoma
- Giant cell granuloma
- Dentigerous cyst
Discussion
After the surgeon reviewed the biopsy report, they counseled the patient. The patient was scheduled a few weeks later for a complete resection of the lesion.
Unicystic ameloblastoma
Ameloblastomas have an epithelial origin and account for 10% to 30% of all odontogenic tumors. Ameloblastomas occur in three different clinico-radiographic situations: conventional solid or multicystic, unicystic, and peripheral (extraosseous).
Unicystic ameloblastomas are benign, slow-growing, and locally aggressive tumors. They are a rare variant of ameloblastomas that usually occur in younger populations. The majority of cases are found in the posterior mandible. The lesion is often asymptomatic, although a large lesion can be symptomatic and may cause some swelling of the mandible.
From the radiographic perspective, unicystic ameloblastomas show expansive unilocular radiolucency with well-defined and well-corticated borders. Root resorption is often present with minimal displacement. The majority of cases are associated with an impacted or unerupted tooth. The differential diagnosis includes dentigerous cyst and keratocystic odontogenic tumor.
The diagnosis is made only after histologic examination. Three different histological variants of unicystic ameloblastomas are recognized: luminal, intraluminal, and mural.
The treatment is complete surgical excision. Recurrence after the surgical treatment is common, with recurrence rates as high as 20%. Patients should undergo long-term follow-up.
Reference
Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 3rd ed. St. Louis, MO: Saunders/Elsevier; 2009.
Answer key:
Odontogenic keratocyst
Unicystic ameloblastoma
Unicystic ameloblastoma