Digital dentistry continues to transform restorative procedures, offering new possibilities for both clinicians and patients.1 While digital workflows have become increasingly common for indirect restorations, their application in direct restorative procedures represents a frontier with significant potential.2 This case study examines the use of 3D-printed direct resin veneers as an innovative alternative to traditional hand-layered composite or porcelain veneers.
 Dr. Michael Morgan.
Dr. Michael Morgan.
The procedure described provides several key advantages: significantly reduced chair time, less physically stressful for the clinician, less need for high-end anterior composite skills, lower costs for patients, minimal tooth preparation, and predictable aesthetic outcomes.2 As digital technologies continue to evolve, 3D-printed direct composite veneers may represent an important addition to the restorative arsenal for addressing anterior aesthetic challenges.3
By leveraging digital facial scanning, intraoral scanning, CAD software, and advanced 3D-printed resin, the case was completed in a fraction of the time required for traditional layered composite or porcelain restorations. The following case study outlines the clinical workflow, material selection, and patient outcomes, highlighting the advantages of 3D-printed restorations in modern aesthetic dentistry.
Patient information and diagnosis
The patient was a 23-year-old man who presented with multiple diastemas between teeth #6-11 resulting from orthodontic relapse (Figures. 1-5). Despite previous orthodontic treatment that had reduced the spaces, complete closure could not have been achieved without surgical intervention. Following the orthodontic treatment, the patient experienced significant relapse after discontinuing the use of his retainers, resulting in spaces between teeth #6-11 and some tilting of teeth.
The patient's primary concern was aesthetics, specifically the gaps between his maxillary teeth. While retreatment with orthodontics was discussed as an option to address the diastemas, the patient declined due to concerns about additional time and cost. The diagnosis was multiple diastemas and bite collapse from orthodontic relapse.4
Treatment planning and material selection
After discussing various treatment options with the patient, the decision was made to proceed with 3D-printed direct composite veneers for teeth #4-13. This approach offered several advantages over alternative treatments. Compared to hand-layered direct composite veneers, which would require 16 to 20 hours of chair time, the 3D-printed approach required only about three hours total (one hour for diagnostics and soft-tissue adjustments and less than two hours for delivery). Additionally, the cost to the patient was approximately half that of porcelain veneers, making the treatment more accessible.
The treatment required minimal enamel-only preparation of four teeth (#7-10), making it less invasive than traditional veneers. Furthermore, the digital design allowed for visualization of the outcome prior to treatment, ensuring patient acceptance and predictable results.5 (Figure 6A).
The primary challenge in this case was achieving proper tooth proportions due to the spacing issues. Without proper planning, direct veneering would have resulted in short, wide teeth for #7-10, creating an unaesthetic appearance (Figures 7 and 8). To address this, a digital workflow was employed to redistribute space and create natural-looking proportions.
Digital workflow
The digital workflow began with comprehensive diagnostic records. This digital information was then used for a digital smile design process, where the intraoral scan and face scan were integrated to show the patient potential outcomes. The design was created using Exocad software, which allowed for visualization of different treatment approaches.
Two options were presented to the patient. Option A involved no tooth preparation and no soft-tissue modification, while Option B incorporated minimal tooth preparation and soft-tissue laser modification. After seeing both options, the patient chose Option B, understanding that the minimal intervention would provide superior aesthetic results (Figures 6-10).
Key design considerations included improving the length-to-width ratios of teeth #7-10.6 The digital design allowed for redistribution of the diastema spaces to create more proportionate teeth.
First appointment: Diagnostics and preparation
The first appointment included comprehensive diagnostics with full photos, digital impressions using the Medit scanner, and face scanning with the MetiSmile system manufactured by Shining 3D. Minimal preparation was performed, including the reduction of 0.75 mm of enamel on the distal surfaces of teeth #8 and #9 and 0.5 mm of enamel on the distal surfaces of teeth #7 and #10.7 Importantly, no preparation was done into dentin or on the facial surfaces of any teeth, and the canines and bicuspids remained completely unprepared. The preparation was performed using a KaVo electric high-speed handpiece with a Brasseler fine chamfer diamond.
Soft-tissue modification was also performed during this appointment. This included gingival recontouring with a Bluewave diode laser from Clinician's Choice to raise the gingival margins on teeth #8 and #9. Additionally, a frenectomy was performed between teeth #8 and #9 to address the low-positioned frenum that was impacting aesthetics. Because of the minimal nature of the preparation, no temporaries were required, which further simplified the process for the patient.
Veneer design and fabrication
Following the initial appointment, the digital design of the veneers was created using Exocad software, with careful attention to proper tooth proportions. The veneers were then printed with OnX Tough 2 Bleach Shade resin using a SprintRay Pro 2 printer, while a solid model was printed on an Einstein printer for verification and finishing.
The post-processing protocol was critical to the success of the restorations. When the veneers emerged from the printer, they were sprayed with 91% alcohol to remove excess liquid resin. The intaglio surface of each veneer was cleaned with 91% alcohol using a microbrush, and the support legs were trimmed from each restoration. The veneers were then placed on the solid model for verification of fit.
A crucial innovation in the protocol was the application of a thin coat of Kuraray Majesty ES Flow on the facial surfaces of each veneer to enhance gloss retention (Figure 10). After application, the veneers were light-cured for five seconds with a Valo Grand curing light from Ultradent, then placed in a SprintRay NanoCure unit for final curing according to material specifications. Following this curing cycle, the veneers were placed in glycerin and cured again in the NanoCure unit to eliminate the oxygen-inhibited layer (Figure 11).8
Second appointment: Delivery
The delivery appointment began with isolation using OptraGate (Ivoclar Vivadent) and Yuyte dental sponge (Yuyte International) as needed to control the operative field. After prophylaxis with nonfluoride paste, a 000 cord soaked in Oraqix gel was placed for patient comfort. The prepared teeth were etched with K-Etchant from Kuraray followed by application of Clearfil Universal Bond Quick 2 (Kuraray), which was air-thinned but not light-cured.9
Preparation of the veneers involved microabrasion of the intaglio surface with aluminum oxide followed by cleaning with Katana Cleaner from Kuraray. Ceramic primer was then applied, followed by Universal Bond Quick 2 (Kuraray), which was air-thinned but not light-cured.
For cementation, Panavia Veneer LC Cement in the soft white shade from Kuraray was used. The veneers were seated in their correct positions, and excess cement was removed with a rubber tip. Each veneer was spot-cured in the center with an Ivoclar Bluephase curing light with a small 2-mm tip to stabilize the restoration while allowing for continued cleanup. After additional cleanup with a rubber tip, glycerin was applied in interproximal areas with floss cleanup to ensure complete removal of excess cement.
Final curing was performed with a Valo Grand curing light from Ultradent for five seconds each from both facial and lingual aspects. This process was repeated four times per tooth (40 seconds total per tooth) to prevent heat buildup while ensuring complete polymerization. Finishing and polishing were performed using a DiaComp Feather Lite gray polisher for high gloss followed by Enamelize from Cosmedent and a goat hair wheel from Clinician's Choice. Finally, lingual occlusion was checked and adjusted as needed to ensure proper function.
Results and discussion
The patient was extremely pleased with the immediate aesthetic outcome (Figures 12 and 13). The 3D-printed direct composite veneers successfully addressed the diastemas while creating natural-looking tooth proportions. The minimal preparation approach preserved tooth structure while still allowing for optimal aesthetic results.10
Several key factors contributed to the success of this case. The integration of intraoral scanning and face scanning allowed for predictable planning and patient visualization of the outcome. The innovative coating technique using Kuraray Cleafil Majesty ES Flow on the external surfaces of the 3D-printed veneers addressed one of the primary concerns with 3D-printed restorations: gloss retention. Previous injection molding cases by the author with this material have shown gloss retention for over three years with no additional polishing, suggesting promising long-term results.
The efficiency gains were substantial, with a total treatment time of approximately three hours compared to 16 to 20 hours for hand-layered composite veneers. This reduction in chair time benefits both the clinician and the patient.11 The cost-effectiveness of the procedure, at approximately half the cost of porcelain veneers, makes aesthetic improvements more accessible to patients. Moreover, I found this approach to be significantly less physically and mentally stressful compared to hand-layered techniques.
Product efficacy and longevity considerations
While 3D-printed restorations are relatively new and lack long-term clinical studies, several aspects of this protocol suggest promising durability.12 The use of Kuraray Clearfil Majesty ES Flow provides a highly polishable outer layer with documented gloss retention. The careful post-processing, including glycerin curing to eliminate the oxygen-inhibited layer, helps ensure optimal physical properties.8
Unlike porcelain, composite restorations are "renewable," meaning the outer layer can be refreshed or refinished if needed. The outer layer can be removed with air abrasion and recoated if the gloss diminishes over time, providing a long-term maintenance option that does not exist with ceramic restorations.
Kuraray Panavia Veneer LC cement in soft white is an outstanding product that simplifies the cementation process. Rather than custom mixing to achieve the desired shade, the premixed soft white provides an ideal balance that enhances veneer appearance without appearing overly bright. This ready-to-use cement exemplifies how material innovations can streamline workflow while achieving optimal results.
Conclusion
3D-printed direct composite veneers represent an innovative approach to addressing anterior aesthetic challenges. This case demonstrates how digital workflows can be leveraged to create minimally invasive, cost-effective, and time-efficient restorations.13 The advantages include reduced treatment time (approximately one-sixth of the time required for hand-layered composites), lower cost compared to porcelain veneers, minimal tooth preparation, and predictable aesthetic outcomes through digital planning.
While the author has enjoyed performing hand-layered composite veneers for 25 years and has learned from talented composite artists worldwide, this more efficient and simpler approach is likely to become increasingly common as digital technology advances. As the technology continues to mature and long-term studies become available, 3D-printed direct composite veneers will become a standard option in the restorative arsenal.
For patients seeking aesthetic improvements who are concerned about cost or the amount of tooth structure removal required for traditional veneers, 3D-printed direct composite veneers offer a compelling alternative. The digital workflow also provides a significant advantage by allowing patients to visualize potential outcomes before committing to treatment, leading to higher satisfaction with final results.
While no restoration is permanent, the "renewable" nature of these restorations provides an additional advantage for long-term maintenance. For the advantages listed previously, 3D-printed direct composite veneers have the potential to replace hand layering as the dominant technique for fabricating and delivering direct resin veneers.
 Figure 1: Pre-op smile.Images and captions courtesy of Dr. Michael Morgan.
Figure 1: Pre-op smile.Images and captions courtesy of Dr. Michael Morgan.
 Figure 2: Close-up of retracted facial view (pre-op).
Figure 2: Close-up of retracted facial view (pre-op).
 Figure 3: Right facial view (pre-op).
Figure 3: Right facial view (pre-op).
 Figure 4: Left facial view (pre-op).
Figure 4: Left facial view (pre-op).
 Figure 5: Close-up of retracted maxillary arch.
Figure 5: Close-up of retracted maxillary arch.
 Figure 6A: Initial design in Exocad discussed with the patient.
Figure 6A: Initial design in Exocad discussed with the patient.
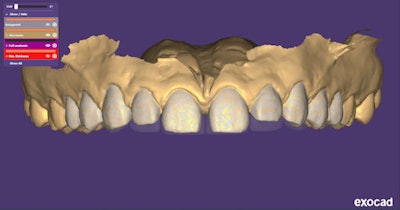 Figure 6: Pre-op digital impression of teeth #4-10.
Figure 6: Pre-op digital impression of teeth #4-10.
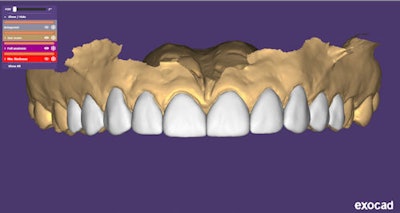 Figure 7: Veneer mock-up -- no prep or soft-tissue changes.
Figure 7: Veneer mock-up -- no prep or soft-tissue changes.
 Figure 8: Digital impression of prepared teeth.
Figure 8: Digital impression of prepared teeth.
 Figure 9: Veneer design -- improved aesthetics with distal preps #7, #8, #9, #10, and soft-tissue changes.
Figure 9: Veneer design -- improved aesthetics with distal preps #7, #8, #9, #10, and soft-tissue changes.
 Figure 10: Facial surfaces of the veneers coated with Kuraray Majesty ES Flow to enhance gloss retention.
Figure 10: Facial surfaces of the veneers coated with Kuraray Majesty ES Flow to enhance gloss retention.
 Figure 11: All of the veneers were placed in glycerin for final curing to eliminate the oxygen-inhibited layer.
Figure 11: All of the veneers were placed in glycerin for final curing to eliminate the oxygen-inhibited layer.
 Figure 12: Immediate post-op with 3D-printed veneers.
Figure 12: Immediate post-op with 3D-printed veneers.
 Figure 13: Post-op smile.
Figure 13: Post-op smile.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.
Dr. Michael Morgan is a world-renowned cosmetic dentist who earned his degree from the University of Illinois School of Dentistry before advancing his expertise in composite aesthetics by studying with some of the world’s premier composite artists across Europe. Morgan has lectured and taught across the U.S., Canada, Europe, and Asia on the latest composite techniques. He maintains a private practice in Hinsdale, IL, focusing on advanced aesthetic outcomes. He is also a founder of VeneerRay.com, providing 3D-printed direct composite veneers to general dentists.
References
- Gawali N, Shah PP, Gowdar IM, Bhavsar KA, Giri D, Laddha R. The Evolution of Digital Dentistry: A Comprehensive Review. J Pharm Bioallied Sci. 2024 Jul;16(Suppl 3): S1920-S1922.
- Revilla-León M, Özcan M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J Prosthodont. 2019;28(2):146-158.
- Rekow ED. Digital dentistry: The new state of the art -- Is it disruptive or destructive? Dent Mater. 2020;36(1):9-24.
- Abraham R, Kamath G. Midline diastema and its aetiology--a review. Dent Update. 2014;41(5):457-464.
- Lin WS, Zandinejad A, Metz MJ, Harris BT, Morton D. Predictable restorative work flow for computer-aided design/computer-aided manufacture-fabricated ceramic veneers utilizing a virtual smile design principle. Oper Dent. 2015;40(4):357-363.
- Magne P, Gallucci GO, Belser UC. Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. J Prosthet Dent. 2003;89(5):453-461.
- LeSage BP. Minimally invasive dentistry: paradigm shifts in preparation design. Pract Proced Aesthet Dent. 2009;21(2):97-101.
- Shawkat ES, Shortall AC, Addison O, Palin WM. Oxygen inhibition and incremental layer bond strengths of resin composites. Dent Mater. 2009;25(11):1338-1346.
- Pashley DH, Tay FR, Breschi L, et al. State of the art etch-and-rinse adhesives. Dent Mater. 2011;27(1):1-16.
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5):503-509.
- Fasbinder DJ. Digital dentistry: innovation for restorative treatment. Compend Contin Educ Dent. 2010;31(Spec No 4):2-11.
- Stansbury JW, Idacavage MJ. 3D printing with polymers: Challenges among expanding options and opportunities. Dent Mater. 2016;32(1):54-64.
- Dawood A, Marti BM, Sauret-Jackson V, Darwood A. 3D printing in dentistry. Br Dent J. 2015;219(11):521-529.



















