Burned-out employees, difficult patients, and running a dental practice may be overwhelming -- even frightening -- but may pale in comparison to what may be seen in the dental chair. In the spirit of Halloween, DrBicuspid reviews 2023’s most hair-raising case reports.
Our top story involves a toddler who had a seizure following a toothbrush injury. The child was left with life-altering complications. Other terrifying reports include the migration of an orthodontic wire, a failed dental prosthetic due to a continuous positive airway pressure (CPAP) mask and machine, temporal muscle ossification due to a local anesthetic injection, and other devastating case reports.
Without any delay, here are the eight most horrifying case reports of 2023.
1. Toothbrush injury causes stroke in 2-year-old boy
A 2-year-old boy experienced a blunt cerebrovascular injury to the pharynx that led to an ischemic stroke following a fall while he was brushing his teeth. After treatment and a lengthy hospital stay, the boy remained paralyzed on the lower half of his body on the left side, according to a clinical note published in Pediatrics International.
2. Orthodontic wire travels to a boy’s brain, causing a seizure
A 12-year-old boy in Texas experienced a seizure after an orthodontic wire from his braces migrated into his temporal lobe.
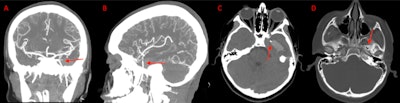 A coronal (A) and sagittal (B) view of the CT angiogram shows the wire penetrating through the skull floor of a 12-year-old boy. (C) An axial view of CT demonstrates the wire in the temporal lobe and the associated intraparenchymal hemorrhage. (D) Axial bone window CT shows the wire entering through the foramen ovale. Images courtesy of Morgan et al. Licensed by CC BY 4.0.
A coronal (A) and sagittal (B) view of the CT angiogram shows the wire penetrating through the skull floor of a 12-year-old boy. (C) An axial view of CT demonstrates the wire in the temporal lobe and the associated intraparenchymal hemorrhage. (D) Axial bone window CT shows the wire entering through the foramen ovale. Images courtesy of Morgan et al. Licensed by CC BY 4.0.
After imaging confirmed the metallic foreign object, which had migrated via the foramen ovale into the temporal lobe, as well as an associated intraparenchymal hemorrhage, the wire was removed without complications. The boy sustained no measurable damage to any structures within or around the foramen ovale, including the carotid artery, which would have been devastating, according to the case report in Radiology Case Reports.
3. Patient develops air in facial vein during crown preparation
On two separate occasions, air blown from a turbine drill became trapped in a major facial vein of a healthy woman during dental crown preparation. This could have threatened her life.
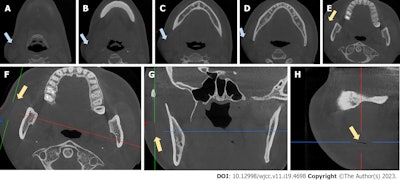 Coronal views of CBCT scans (A-E) show swelling. The CBCT scan shows an air-filled fissure between the masseter muscle and soft tissue (F-H) . The blue arrows indicate swelling, while the yellow arrows indicate the fissure. Images courtesy of Sun et al. Licensed by CC BY 4.0.
Coronal views of CBCT scans (A-E) show swelling. The CBCT scan shows an air-filled fissure between the masseter muscle and soft tissue (F-H) . The blue arrows indicate swelling, while the yellow arrows indicate the fissure. Images courtesy of Sun et al. Licensed by CC BY 4.0.
Fortunately, the woman’s prompt diagnosis and treatment prevented cervical subcutaneous emphysema in the angle of the retromandibular vein from developing into a deep space infection, air embolism, cranial nerve palsy, or worse, according to a report published in the World Journal of Clinical Cases.
4. Local anesthesia led to temporal muscle ossification
A healthy woman developed the extremely rare complication of traumatic myositis ossificans of the temporal muscle attachment after receiving an injection of local anesthesia for root canal treatment.
 The (A) panoramic x-ray after surgical treatment shows partial resection of the lesion and the coronoid process (arrow). A (B) clinical image of the resected lesion. Images courtesy of Pedersen et al. Licensed by CC BY 4.0.
The (A) panoramic x-ray after surgical treatment shows partial resection of the lesion and the coronoid process (arrow). A (B) clinical image of the resected lesion. Images courtesy of Pedersen et al. Licensed by CC BY 4.0.
Following the dental procedure, the woman experienced persistent limited mouth opening. Eventually, she made a full recovery after undergoing a coronectomy and engaging in physical therapy and regular jaw exercises, according to a report published in Clinical Case Reports.
5. CPAP use may have led to man’s dental implant prosthesis failure
The use of a CPAP mask and machine may have led to a 71-year-old man’s dental prosthesis failure, highlighting this sleep apnea therapy as a possible high-risk factor for implant failure.
Until the immediate failure of the man’s full-arch implant prosthesis, there have been no reported cases of CPAP machine usage as a risk factor for implant failure. After the failure, the man stopped using the CPAP machine for three weeks as instructed by clinicians, and a revision implant surgery was successfully completed, according to a report published in the Journal of Prosthodontics.
6. Rubber dam clamp may lead to cortical tooth necrosis
A stainless-steel rubber dam clamp used during a root canal may have led to cortical necrosis in a healthy 22-year-old woman's mandibular tooth.
The report, which was published in the Journal of Endodontics, was believed to be the first published report showing the effect that a rubber dam clamp may have on underlying bone in healthy patients. After a rubber dam clamp is removed following a dental procedure, clinicians should document the position of the tooth isolation brace and evaluate alveolar tissues.
7. Acne gel may have triggered anaphylaxis in oral surgery patients
Two teens who previously used antibiotic topical acne gels experienced anaphylaxis following administration of IV clindamycin prior to third-molar surgeries, according to a case report published in Oral Surgery.
Prior to their surgeries, both patients had only previously been exposed to clindamycin via topical acne gels, which may have primed their immune systems for anaphylaxis when they internally received the antibiotic.
8. Local anesthesia may be linked to woman’s tongue paralysis
A 64-year-old woman in Tennessee experienced tongue paralysis, which affected her ability to talk, following the administration of local infiltration anesthesia for a dental restoration procedure. The case report was published in Oral and Maxillofacial Surgery Cases.
 The woman's tongue shows right-sided atrophy and mild right-sided deviation. Image courtesy of Scott et al. Licensed by CC BY 4.0.
The woman's tongue shows right-sided atrophy and mild right-sided deviation. Image courtesy of Scott et al. Licensed by CC BY 4.0.
Within a few months, the woman mostly recovered from the injury of her hypoglossal nerve, the 12th cranial nerve that is responsible for stimulating almost all intrinsic and extrinsic muscles of the tongue. Her injury could have been caused by mechanical compression during local infiltration, which compressed the nerves; a chemical injury related to the local anesthetics that were used; or direct injury by the needle, the authors surmised.